What’s the difference between Premenstrual syndrome (PMS) and Premenstrual dysphoric disorder (PMDD)?
In this article
What's the lowdown?
PMS symptoms vary from person to person, you may not experience them all, or at the same intensity as others. PMDD is a severe form of PMS that has a significant impact on daily functioning.
To be diagnosed with PMDD you must have 5+ symptoms, including one mood-related symptom, e.g. mood swings, feelings of sadness or anxiety.
Scientists aren’t actually 100% clear about exactly what causes PMS and PMDD, but there are a few theories as to why it happens.
Some people are advised to take the combined contraceptive pill continuously for management of pain and other symptoms. This works for some because it levels out the hormonal fluctuations experienced throughout the menstrual cycle.
Talking therapies and antidepressants could help to manage the severe symptoms of PMDD alongside pain relief. Before going to your GP, make sure to track your symptoms over a few months for reference.
Life’s a funny thing; one week you’re on top of everything, clear-headed and totally fine, the next you’re weeping because you stood on a snail in the car park of Asda.
Introducing PMS, the monthly friend of millions of women and people who menstruate. It’s responsible for the symptoms you may notice before your period – whether physical or mental – and the severity of its impact varies from person to person.
On the lower end of the spectrum, you might experience bloating and light mood swings. At the other end is PMDD (Premenstrual Dysphoric Disorder), which can have a significant impact on the ability to carry out normal life and activities.
Here we’ll dive deep into both conditions, looking at the symptoms, possible causes and treatments. We’ll also answer the question: can contraception help?
Think this blog will be useful? Check out our newsletter for more:
Symptoms of PMS and PMDD
Premenstrual Syndrome (PMS) is an umbrella term for a variety of symptoms you may experience in the days or weeks leading up to your period. The most common include:
- Bloating
- Cramps
- Breast tenderness
- Mood swings (feeling more upset, angry, anxious or irritable)
- Spots and greasier skin
- Greasy hair
- Headaches
- Tiredness or insomnia
- Appetite changes
- Reduced or heightened sex drive
Not everyone experiences all of these symptoms, and they vary in intensity from person to person. Some will recognise their own combination of signals that tell them their period is due; and some months these might be intense, while others you may barely notice them. The lucky ones might not get any symptoms at all (#blessed).
Premenstrual Dysphoric Disorder is a severe form of PMS, and is a diagnosable condition. It has more severe symptoms and a significant impact on daily functioning. It affects around 1 in 20 women.
Symptoms occur a week or two before your period starts and generally subside a few days after the start of your period. Symptoms include:
- Lasting irritability or anger that may affect other people
- Feelings of sadness or despair, or even thoughts of suicide
- Feelings of tension or anxiety including tingling in the hands and feet
- Panic attacks
- Mood swings or crying often
- Lack of interest in daily activities and relationships
- Trouble thinking or focusing
- Tiredness or low energy
- Food cravings or binge eating
- Trouble sleeping
- Feeling out of control
- Physical symptoms such as cramps, bloating, breast tenderness, headaches, and joint or muscle pain
To be diagnosed with PMDD you must have 5+ symptoms, including one mood-related symptom, e.g. mood swings, feelings of sadness or anxiety.
What causes PMS and PMDD?
Scientists aren’t actually 100% clear about exactly what causes PMS and PMDD, but there are a few theories as to why it happens.
Hormonal changes
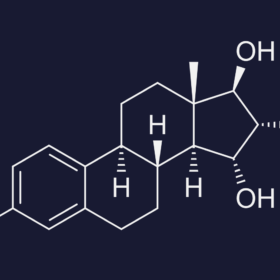
Hormones follow a cycle – they ebb and flow throughout the month, and your mood and body responds accordingly. After ovulation, and before your period begins, oestrogen and progesterone rise. Higher levels of these hormones can cause anxiety, irritability and mood swings. Once your period begins, these hormones drop off, and symptoms of PMS or PMDD tend to disappear.
One very small study looked at 18 women who had been diagnosed with PMS. They found that those with higher levels of oestrogen and progesterone during the luteal phase of their cycle (the time after ovulation but before a period) had more severe symptoms of PMS and lower mood.
What isn’t clear, however, is whether one of these hormones is more responsible for PMS or PMDD symptoms than the other. The science suggests that progesterone might be the main culprit, but this doesn’t necessarily mean that higher progesterone equals stronger symptoms. The more likely answer, according to research, lies in how and when progesterone levels are high in the body.
A study from the 90s found that progesterone was necessary early after ovulation for PMS to occur, while more recent research suggests that people with severe PMS or PMDD experience a sharp drop in progesterone in the final days before their period. Those without PMS symptoms, in comparison, had a slow and gradual decline in progesterone during this time.
It’s also true that some people who menstruate are simply more sensitive to hormonal changes than others. If you’ve ever reacted badly to a new contraceptive pill that everyone else seems to love, you know what we mean.
Changes to brain chemistry
There is a chemical in your brain called serotonin, and it interacts with lots of different parts of your body all the time. It is thought that one of its roles is to regulate your mood and emotions; contributing to happiness and keeping anxiety and low mood in check.
In people experiencing PMS or PMDD, serotonin drops as oestrogen drops at the end of the luteal phase of the menstrual cycle just before your period starts. Some scientists think, then, that this reduction in serotonin can impact your mood and be responsible for the emotional symptoms of PMS and PMDD.
It is also thought that women with major depression are more susceptible to PMDD than those who have moderate or no depression.
Essentially, we still don’t have a definitive answer as to why PMS and PMDD occur. Oestrogen, progesterone and serotonin are all thought to play a role, but it is difficult to tease apart the effects of each.

Can contraception help with PMS and PMDD?
For some, yes. Research has found that newer types of combined contraceptive pill, which contain drospirenone, can improve PMS symptoms. For those suffering with PMDD, the research is encouraging, and suggests it could help in some cases.
This type of pill may be the first treatment most people who menstruate are offered when they see their doctor about PMS or PMDD, and they may be advised to take it continuously to improve symptom management.
The pill works for some people because it levels out the hormonal fluctuations we experience throughout our cycle. With progestogen and oestrogen spikes both being potential culprits for the symptoms some of us experience before our periods, it makes sense that ironing these out could have an impact on how we feel. The pill prevents ovulation (and therefore the subsequent hormone spike), and when it’s taken continuously, oestrogen and progestogen won’t suddenly drop before your withdrawal bleed in your pill free week, which might lessen PMS or PMDD symptoms.
Unfortunately, there’s no umbrella treatment for PMS or PMDD, and a contraceptive pill that works for one person may not work for another.
What about other methods that stop ovulation?
You might be wondering about progestogen-only contraception, like the mini pill, injection or hormonal coil. They can also stop ovulation, so it would make sense that they could have the same effect, right? Well, maybe not.
Progestogen-only contraception can alter the way you bleed each month. Some people may stop bleeding altogether, while others might experience spotting or irregular bleeding. It may be that progestogen-only contraception, if it stops periods altogether, may help PMS in some individuals but it can also reproduce symptoms in others. Progesterone or progestogens or therefore not considered suitable treatment for PMS symptoms.
So what’s the best contraceptive pill for PMS and PMDD?
Yasmin, Lucette, Eloine and Drovelis are all contraceptive pills containing synthetic oestrogen and drosperinone, which is thought to improve PMS and PMDD symptoms. You can now buy Yasmin and other contraceptive pills here at The Lowdown.
Can contraception make PMS or PMDD worse?
While some find that contraception improves their symptoms, others find that it actually makes them worse. Some side effects of contraception, like bloating, breast tenderness and cramps, are also the symptoms of PMS and PMDD, so it can be hard to tease apart the two.
When it comes to mood symptoms of PMS and PMDD, the effect of contraception is also unclear. One study of 658 women taking oral contraception found that more reported a deterioration in PMS symptoms than an improvement. On the other hand, a study of almost a thousand women in Southampton found that use of hormonal contraception was associated with a lower prevalence of PMS symptoms.
Annoyingly, there still doesn’t seem to be an answer as to whether hormonal contraception in general improves or worsens PMS or PMDD. This is perhaps because there never will be an answer; as frustrating as it is, everyone is different, and our sensitivity to hormonal changes, as well as the unique balance of hormones in our bodies, mean that we will all react differently.
If you’d like to discuss contraceptive options for managing PMS or PMDD, The Lowdown offers online consultations with their medical team; essentially a 20 minute chat with a professional who specialises in contraception, who can talk you through your options and create a personalised action plan.

Is there anything else that can help with PMS or PMDD?
If you’re here because you suffer with PMS or PMDD and are looking for answers, you’ve probably heard the ‘diet, exercise, lots of sleep’ advice a thousand times. We all know that these things are good for us, but sometimes they’re not enough. The NHS has a great page about lifestyle adjustments you can make, but if your symptoms persist, it’s time to see your GP.
Pain relief
For light, physical PMS symptoms you may want to try at-home pain relief such as paracetamol or ibuprofen.
Cognitive Behavioural Therapy (CBT)
You may want to discuss CBT with your health professional. This is a talking therapy which can help you to manage PMS symptoms and to address the emotional and psychological side of what you’re going through. It should be offered to everyone with severe PMS. You can access this through your GP on the NHS. Alternatively ThinkCBT is an expert online and in person CBT therapy organisation. They work with many NHS organisations, as well as privately. You can use the access code ‘LowDown’ for a discount.* ;
Antidepressants
You may also be prescribed low dose antidepressants called selective serotonin reuptake inhibitors (SSRIs). Remember we talked about serotonin and its potential role in PMS? These could help to regulate the levels of serotonin in your brain and may work to alleviate the psychological symptoms of your PMS or PMDD. Your GP can discuss the option of taking these every day or just in the lead up to your period.
Before visiting your GP
You might want to keep a symptom diary over a few months, alongside tracking your menstrual cycle, and bring this with you to your GP appointment or Lowdown consultation. This will help your doctor to understand whether you have PMDD, or whether you need help for PMS.
There are a few useful and free apps you can download to track your symptoms easily:
If you prefer to use a pen and paper, there is also a pre-prepared sheet you can print off called the Daily Record of Severity of Problems. You may also find this Self-Screen Tool useful if you’re unsure of your symptoms, but you should always seek help from a professional if you’re at all concerned.
If none of the above treatment options work, you may be referred on to a specialist who can better assess your needs.
If you would like to know more or need support, check out the National Association for Premenstrual Syndromes, International Association of Premenstrual Disorder, Mind Website, and UK PMDD Support Group.
*We have a relationship with this brand so may get a small introducer fee if you use this link
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.