Can you take Yasmin while breastfeeding?
Firstly, congratulations on your new arrival and well done for breastfeeding!
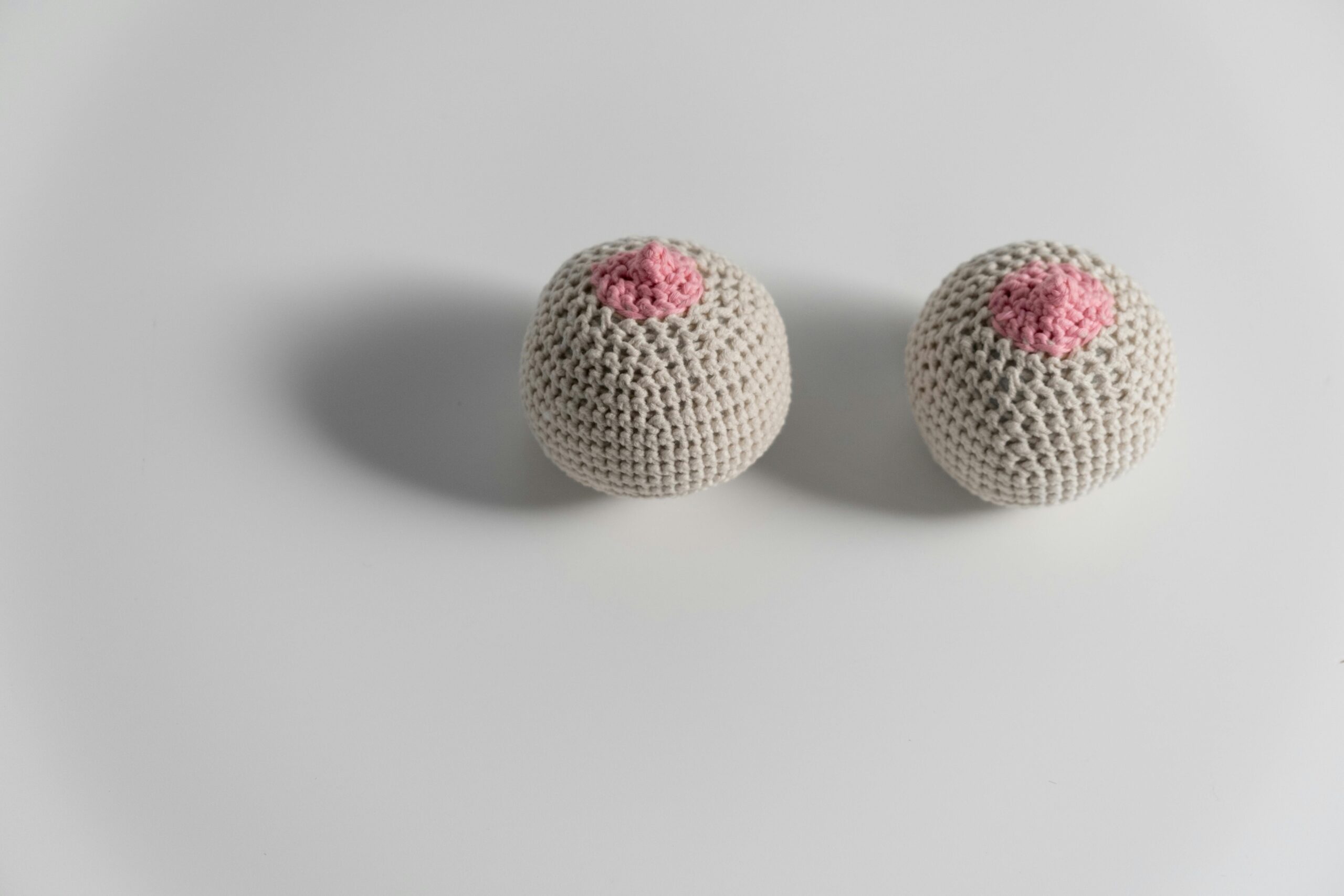
Breastfeeding can be both an amazing, bonding experience but also a difficult journey requiring hard work, determination and luck. While you’re awake all hours of the day and applying barrier cream liberally to your nipples, you’re probably not thinking about a) sex or b) another pregnancy. However, as research suggests that at least a 12 month gap between pregnancies is preferable for both mothers and babies¹,², it’s a good idea to start thinking about your contraceptive options early.
Is Yasmin safe to take while breastfeeding?
The Yasmin pill is one of The Lowdown’s most popular contraceptives. It is a combined pill containing both oestrogen and progestogen. Its popularity may be due to its additional non-contraceptive benefits including treatment for acne, heavy periods and PMS / PMDD. As a new parent, you may be worried about the implications of any new contraceptive on both your and your baby’s health.
For anyone thinking about a combined contraceptive, your medical history needs to be reviewed to check the method is safe for you. Certain personal characteristics such as your BMI, smoking history and a history of blood clots in yourself or a family member can mean combined contraceptives (like Yasmin) are less safe for you. This is due to the small increased risk of blood clots and cardiovascular disease that may be associated with combined contraception for some users. You can speak to your healthcare professional or speak to a doctor at The Lowdown for an insight into your own risk. Yasmin can interact with certain medications so it is important to let us know what other medications you take if you order the pill online.
The risk of blood clots is increased during pregnancy and in the first few weeks after giving birth. Yasmin can be started from 6 weeks after birth if you are breastfeeding and have no other risk factors for blood clots.4 Some women may choose to delay this start to 6 months after birth when the risk of blood clots becomes even lower.
Yasmin should not be started before 6 weeks after birth if you are breastfeeding.4 This is because in addition to an increased blood clot risk in the first few weeks after birth, some research studies suggest that combined pills including Yasmin may reduce weight gain in infants if started within 6 weeks after birth. If Yasmin is started 6 weeks after birth or later, research shows there is no effect on your baby’s weight gain and Yasmin does not affect your baby’s health or development.4
If you are not breastfeeding, Yasmin can be started as early as 3 weeks after birth, as long as you do not have any further risk factors for blood clots.
Yasmin can be taken continuously while breastfeeding and you can even order Yasmin online to avoid the baby brain moments of running out.
Does Yasmin affect milk supply?
Hormonal contraceptives can be found in breastmilk, but in very small amounts (less than 1/100th of the mother’s dose). This has led to worried parents and concerns that contraceptives which contain oestrogen, such as Yasmin, may affect breastfeeding and milk supply. The most recent scientific research is thankfully more reassuring.
Large research studies have shown no significant difference in breastmilk composition, breastfeeding duration and infant growth between users of combined birth control and non users.5
A summary of the scientific literature agrees that previous research indicates combined contraceptives such as Yasmin do not affect milk supply and breastfeeding outcomes overall when started 6 weeks after delivery6,7. When combined pills are started 6 weeks or later after birth, your milk supply is established. A minority of women may experience a drop in milk supply in the first month after starting a combined pill, but this is usually a transient effect. On balance, there is no evidence it affects your baby’s growth. The study also suggests that combined pill brands with an oestrogen content of 30 micrograms or less (such as Yasmin) are better choices to maintain your milk supply while breastfeeding.
If you have any concerns about supply or breastfeeding during your journey or after starting a contraceptive, speak to your health visitor, infant feeding team or a lactation consultant who can offer specialised advice.
What other methods of contraception can you take while breastfeeding?
Breastfeeding itself can be used as a contraceptive, which is known as the lactational amenorrhoea method (LAM). To use LAM correctly, the rules need to be strictly followed and there is research suggesting that the method is less effective in working mums3. We’re unsure how many women use the LAM method worldwide, but often women prefer to choose another reliable method.
Breastfeeding does not limit your contraceptive choice and the majority of options can be started straight after birth. Combined contraceptives such as the combined pill, patch or ring, need to be started later at 6 weeks after birth. The progestogen only pill, injection and implant can be started any time after birth and coils can be inserted within the first 48 hours, or after 4 weeks. As always, your personal medical history should be checked before starting any form of contraceptive to make sure it is safe for you. You can read more details about your options in our blog contraception while breastfeeding.
Contraceptive choice is personal and you shouldn’t feel like you have to use the same method as before your pregnancy. We know that raising a child is hard work, which for example, may affect how easy it is to remember to take a daily pill. Furthermore, anecdotally from Lowdown users, the side effects you experience from a method that was previously really well tolerated before you conceived may alter after pregnancy. If you’re thinking of making a change, use our recommender tool to find the best contraception method for you.
As always, don’t suffer with side effects and chat to one of our doctors for specialised advice.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.