Blood clots and birth control – what are the risks?
Doctors use the blanket term venous thromboembolism (shortened to VTE) to refer to blood clots that form in deep veins (deep vein thrombosis) – often in the leg – and for blood clots that dislodge and travel to blood vessels elsewhere in the body – such as the lungs (pulmonary embolism)2.
If a blood clot blocks an artery it can prevent blood reaching important organs. In worst case scenarios this can result in long term, irreversible damage, or death.
Which all sounds pretty scary.
What causes blood clots in birth control?
Most forms of contraception use the hormones oestrogen and progestin, also known as progestogen. Hormones are chemicals produced by the body to regulate different processes, and researchers have known since the 1970s that there is a relationship between contraception containing synthetic oestrogen and blood clots.
While the exact mechanism isn’t known, research suggests that oestrogen reduces the body’s ability to regulate clotting, making the blood less able to stop forming clots even when it’s not the right time or place.
More specifically, oestrogen appears to dull the body’s sensitivity to an enzyme (a protein that speeds up a biochemical process) called activated protein C (APC). APC downregulates clotting, which means it acts to slow or stop the blood clotting process in response to the body’s needs. With the body less sensitive to APC, the blood is less able to stop clotting.
Research studies have shown higher levels of APC resistance in people taking the combined pill compared to those who are not taking the pill3,4,5.
Before we continue, let’s take a moment to talk risk.
What do we mean by increased risk?
Whenever we read about increased risk, it’s important to know what the baseline risk is. In this case, the baseline risk is the risk of developing a blood clot if you are premenopausal, not pregnant, and not taking any form of birth control. If we tracked 10,000 such women for a whole year, we would expect between two and six of them to develop blood clots6. Put another way, that’s less than 0.1% per year. This baseline risk is so low that increasing it several times over will still result in a very small overall risk for most people.
However, even a small risk can be a cause of concern if you have other risk factors for blood clots, such as a family history. That’s why it’s so important to let your healthcare professional know about your medical and family history before making decisions about your birth control.
Armed with knowledge of the baseline risk, let’s look at different types of contraception.
What is the increased risk of blood clots for different birth control methods?
Combined oral contraceptives
- The combined pill is made up of oestrogen and progestin.
- The risk of developing blood clots when taking the combined pill is between 2 and 5 times higher than the risk of blood clots in women who do not take the pill7,8.
- Progestogens (also called progestins) are a synthetic hormone used in all hormonal contraceptives. There are several types of progestin that have slightly different chemical makeups, but they all work in similar ways.
- We know that progestins on their own do not appear to increase the risk of blood clots, but research has shown that in the combined hormonal contraceptives, different types of progestin used alongside oestrogen seem to have different effects on blood clot risk.
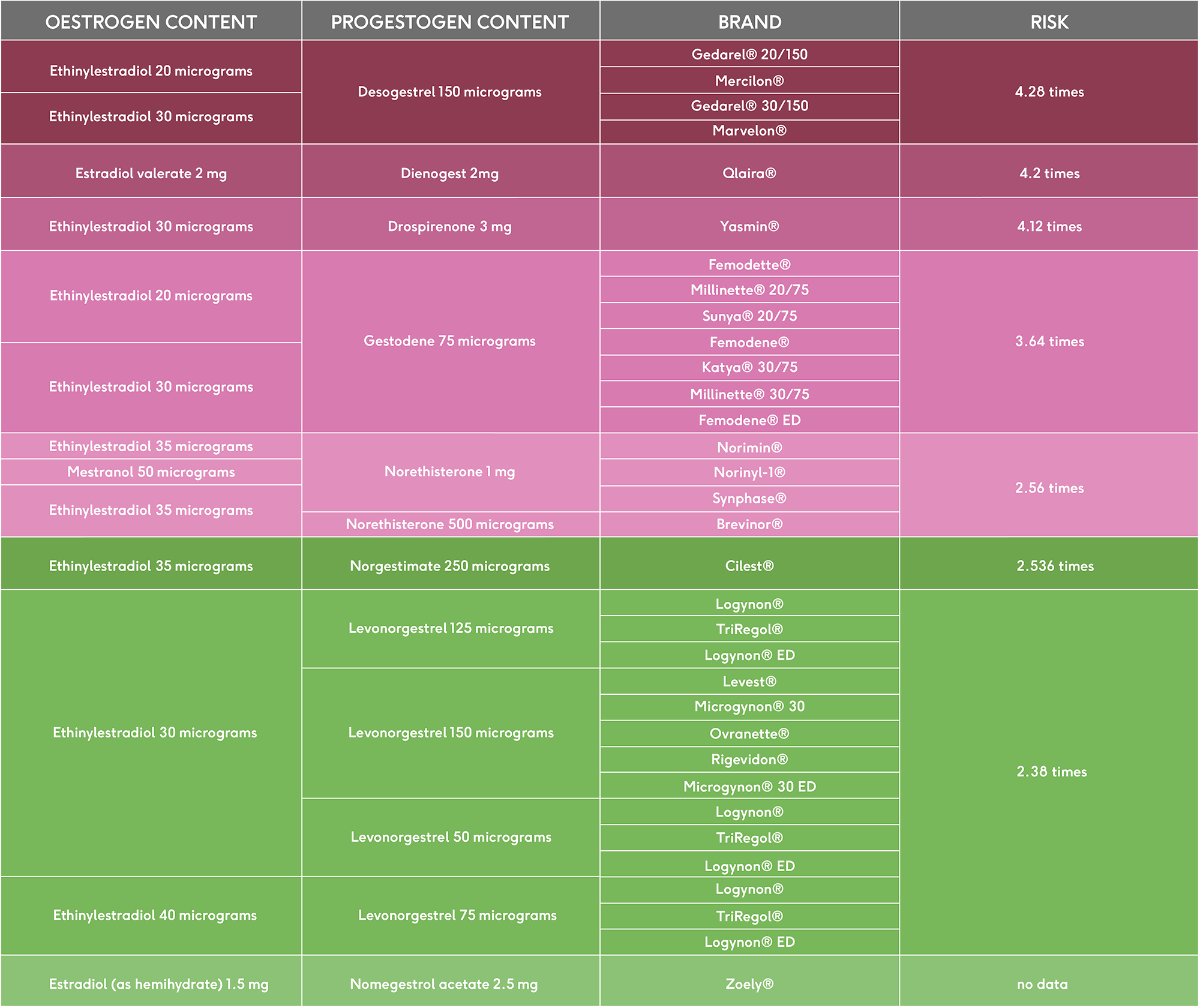
Different types of combined pill and blood clot risk
- A study from 20159 investigated this risk a little further, and found differences depending on the type of progestin used in the birth control pill.
- This large Dutch study that looked at health data from thousands of women aged 15-49 across the Netherlands who had had a blood clot for the first time. They looked at the types of contraceptive they used, if any.
- The research, which has been replicated, showed that different types of progestin used in the combined oral contraceptive pill seem to result in different risk levels for blood clots. It is not yet known why, but it may be to do with how some older progestins counteract the unwanted effects of oestrogen on the clotting process, while newer forms of progestins do not.
- You can see below which types of progestin are associated with an increased risk of blood clots when used in the combined oral contraceptive pill, and which brands contain these different types.
- Taking a combined pill containing a type of progestin called levonorgestrel resulted in the lowest increase in blood clot risk, while pills containing cyproterone acetate present the biggest increase in risk.
- The majority of women in the UK already take a combined pill containing the lower risk combination with levonorgestrel10, and pills with other types of progestin are usually only offered when additional health needs are present, such as severe acne.
- For example, the Yasmin contraceptive pill has a slightly higher blood clot risk compared to other combined pills.
You can view each combined pill ingredients on our product pages. For example, the Microgynon contraceptive pill.
The patch and the vaginal ring
- Much less research has been conducted into blood clot risk with the patch and vaginal ring.
- The patch contains oestrogen. It does appear to increase blood clots risk, and a large Danish study14 found that this risk was just over twice the risk of the oral combined pill.
- The vaginal ring also contains oestrogen, and research suggests it, too, increases blood clot risk15. In the same Danish study, researchers found the risk was just under two times the risk of the oral combined pill.
- The NHS currently advises against use of the patch or the ring where a woman has a history of blood clots16,17.
- More research is needed to understand more fully the risk of blood clots associated with both of these forms of contraceptive.

Progestogen-only pill and the implant (Nexplanon)
- Current evidence suggests that progestogen-only pills (like the Hana mini pill) does not increase the risk of blood clots in healthy women.
- The progestogen only implant also does not increase the risk of blood clots in healthy women11,12,13.
- This is why progestogen-only forms of hormonal contraception are often offered as an alternative to the combined pill for women with increased risk of blood clots.
The hormonal and copper coils
- There is relatively little published research into the hormonal (progestin releasing) IUS or copper IUD and blood clot risk, but it is currently understood that neither increase the risk in healthy women18,19.
This table summarises the risk of blood clots for every method of contraception:
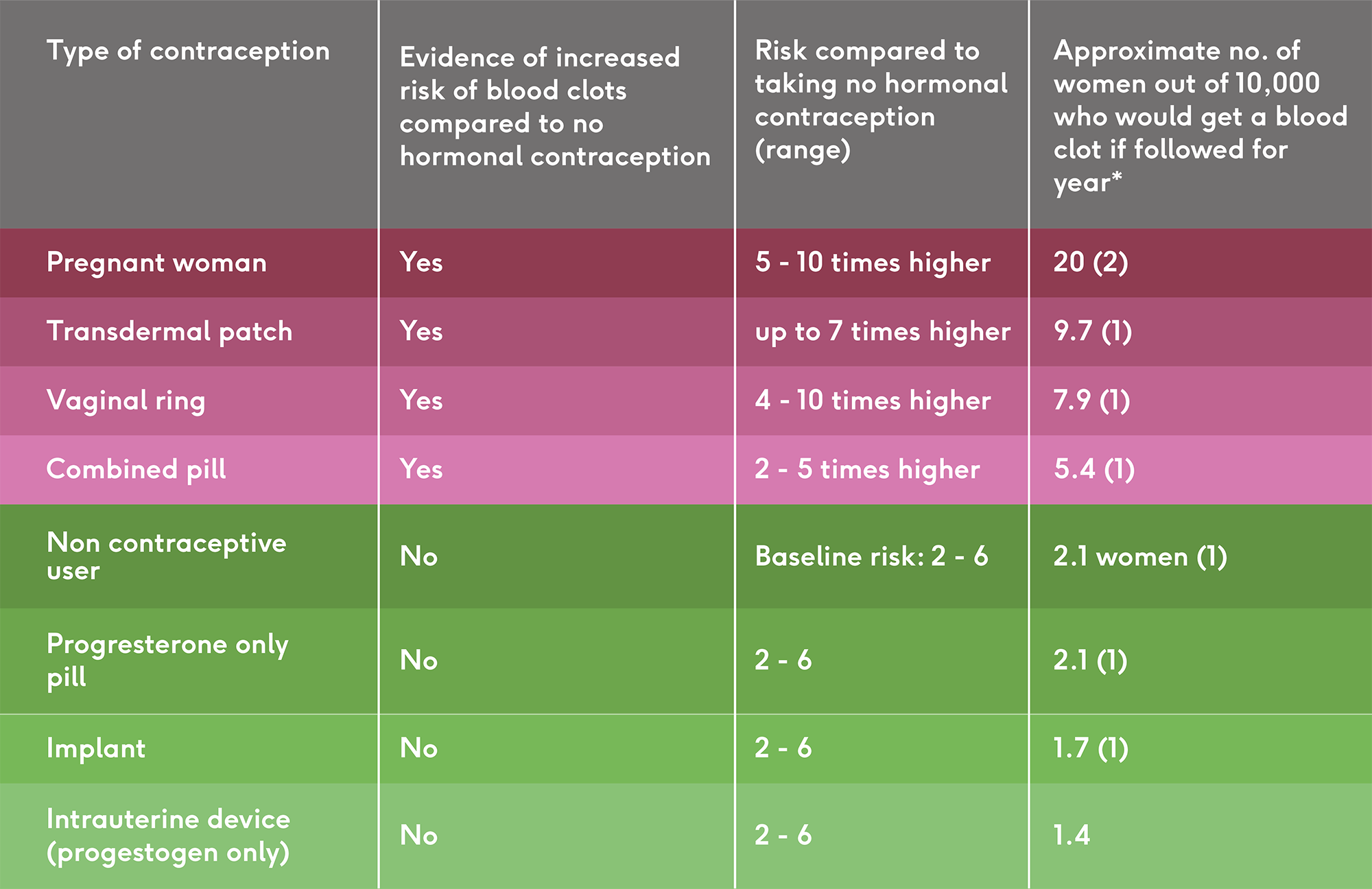
Statistics taken from the following studies 1) Venous thrombosis in users of non-oral hormonal contraception: follow-up study, Denmark 2001-10 & 2) The epidemiology of venous thromboembolism
Should you be worried about blood clots on the pill
- For most women, the increase in the risk of blood clots from hormonal contraceptives doesn’t present a concern.
- Because blood clots are a much higher risk during pregnancy – four to five times the baseline risk20,21 and even higher in the first 6 weeks after giving birth, the consensus in the medical profession is that taking the combined pill is safer than pregnancy.
- However, if you have a family history of blood clots or a condition that predisposes you to blood clots (such as sickle cell anaemia, or thrombophilia), it’s really important that your healthcare professional knows this before you decide on the best form of contraception.
What are the signs of a blood clot?
- Throbbing or cramping pain in the leg or arm
- Swelling, redness and warmth in a leg or arm
- Sudden breathlessness, sharp chest pain (may be worse when you breathe in) and a cough or coughing up blood
Find out more about symptoms and what to do if you think you have a blood clot on the NHS website.
In summary
- Blood clotting is a vital process that prevents excessive bleeding, but if clots form when and where they are not supposed to, the results can be very dangerous.
- The baseline risk of blood clots is so low that increasing it several times over will still result in a very small overall risk for most people.
- Different contraceptive methods have different risks for blood clots. Women taking the combined pill have between a 2 and 5 times higher risk of blood clots compared to women who do not take the pill. Progestogen-only methods do not increase the risk of blood clots.
- For most women, a small increase in risk of blood clots isn’t a concern, but if you have a family or medical history that predisposes you to blood clots the combined risk becomes much higher.
- A contraceptive discussion with your GP or healthcare professional should always cover your family and medical history.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.