What is the best contraception for endometriosis?
In this article
What's the lowdown?
Endometriosis is a complex condition that affects the quality of life of many women
Hormonal contraception is a treatment option to relieving the symptoms of endometriosis
The copper coil is not recommended for endometriosis as it can worsen painful and heavy periods
But many of us still don’t really understand what endometriosis is – and how to treat it. Our in-house GP and Medical Director, Dr Fran shares everything you need to know, including how contraception can help.
What is endometriosis?
Endometriosis is a common health condition, which affects 1 in 10 women of child bearing age. That’s 1.5 million people in the UK.
In endometriosis, cells similar to those usually found in the lining of the womb, grow in other parts of the body. These are called “endometrial deposits” and they can be found on the ovaries, bladder, bowels, pelvic and abdominal walls and in rare cases, even places like the lining of the lung.
As your body moves through its natural menstrual cycle, the womb lining thickens to create a nice home for a potential fertilised egg, before shedding and bleeding if no pregnancy occurs.
The symptoms are really variable for each woman, and not necessarily related to how severe or how many endometrial deposits there are. Symptoms can also be very vague and overlap with other common problems such as IBS (irritable bowel syndrome) or pelvic infections. The main symptoms women complain of are terribly painful periods that interfere with their quality of life.
It is very frustrating for every endometriosis sufferer and those of us who treat it, that we don’t exactly know how or why the condition happens. There are theories, but nothing has been scientifically proven.
One theory called “Retrograde Menstruation” suggests that during a period some of the womb lining travels the wrong way up the fallopian tubes and ends up depositing in the pelvis or abdomen. Another called “Metaplasia” suggests that some cells in the body are able to change to cells found in the womb lining in response to inflammation or certain toxins.
We have seen some research that shows endometriosis can run in families and there could be a genetic factor.
The average time it takes for a woman to receive a definitive diagnosis of endometriosis is 7 years from when symptoms begin. We completely understand this leaves women feeling fed up, exhausted and perhaps even losing trust with the healthcare system.
The “gold standard” for diagnosing endometriosis is via a laparoscopy. This is a small key hole operation in which a camera is inserted into the abdomen and pelvis to look for endometrial deposits. If these are found, they may be treated at the same time.
There are multiple treatment options for endometriosis, one of them being hormonal contraception so let’s dive further into this topic. We went on a quick whistle stop tour of endometriosis, but there is so much more to this complex topic. We have dedicated blogs on endometriosis bloating, endometriosis fatigue, endometriosis fertility and more faqs.
Okay… so what is adenomyosis?
Adenomyosis is a condition where the tissue that lines the inside of the womb can be found deep in the muscle of the womb. This causes problems as it bleeds cyclically and causes pain within the muscle of the womb. It can affect up to 1 in 10 people with a uterus. Symptoms include heavy painful periods and heaviness or discomfort deep in the pelvis.
How can contraception help endometriosis symptoms
Combined hormonal contraceptives thin out the womb lining, prevent ovulation, lighten or even stop periods. This means that endometrial deposits can become smaller without the hormonal stimulation of the menstrual cycle.
Taking the combined pill in a continuous method could offer the greatest relief in symptoms by minimising the number of bleeds you have a year. Find out more about continuous pill taking. These benefits often lead to an improvement in symptoms and can reduce inflammation and scar tissue.

Mirena coil and endometriosis: does it help?
Yes it does too! The hormonal IUS also thins out the womb lining and typically your periods are 90% lighter. 20% of women who use the Mirena coil (a brand of hormonal IUS) will have no periods at all after 12 months, hopefully practically resolving those endometriosis symptoms experienced around period time.
Which is the best birth control for endometriosis?
Any hormonal contraceptive can be beneficial for endometriosis.
At The Lowdown, we believe contraceptive choice should be individualised based on your preferences and desire to avoid certain side effects. But here are some facts that may help you make your decision.
- Research has shown that combined hormonal contraceptives and the IUS can be used as treatment for endometriosis and are equally effective at improving symptoms
- The progestogen-only pill, implant and injection such as Sayana Press also help symptoms, but aren’t considered the “first line treatment” as there has been less research into these methods
- Scientific evidence demonstrates that combined hormonal contraception can prevent endometrial deposits from returning after surgical treatment
There is one rule I have for endometriosis sufferers, and that is to not use the copper coil (IUD). This is because its side effects include longer, heavier and more painful periods, and we don’t want bleeding from those endometrial deposits outside the womb to be longer, heavier and more painful!
You may choose to start hormonal contraception to relieve your symptoms even before a diagnosis is formally made, and this often happens in day to day life.
If you choose to wait for diagnosis and treatment via a laparoscopy, specialists recommend starting hormonal contraception as soon as possible after surgical treatment. Options such as the hormonal IUS could even be inserted at the time of your surgery while you are under anaesthetic if you discuss this beforehand.
As to which hormonal contraceptive is best for you, it really is your choice. The National Institute for Health and Care Excellence (NICE) also has a fantastic resource which I often share with patients to help you make a decision.
They have a nicely laid out table which takes you through several considerations like how your contraceptive choice can affect your periods, the potential side effects, its contraceptive effectiveness and how long it will take for your fertility to return after removal. These are all key aspects to think about before embarking on a contraceptive journey.
Can a copper IUD make endometriosis worse?
A common side effect of the copper IUD is heavier and more painful periods. This would just worsen endometriosis pain, providing no relief for the pain. It also has no hormonal benefits of lightening or stopping periods. This is why the copper coil is not recommended for endometriosis
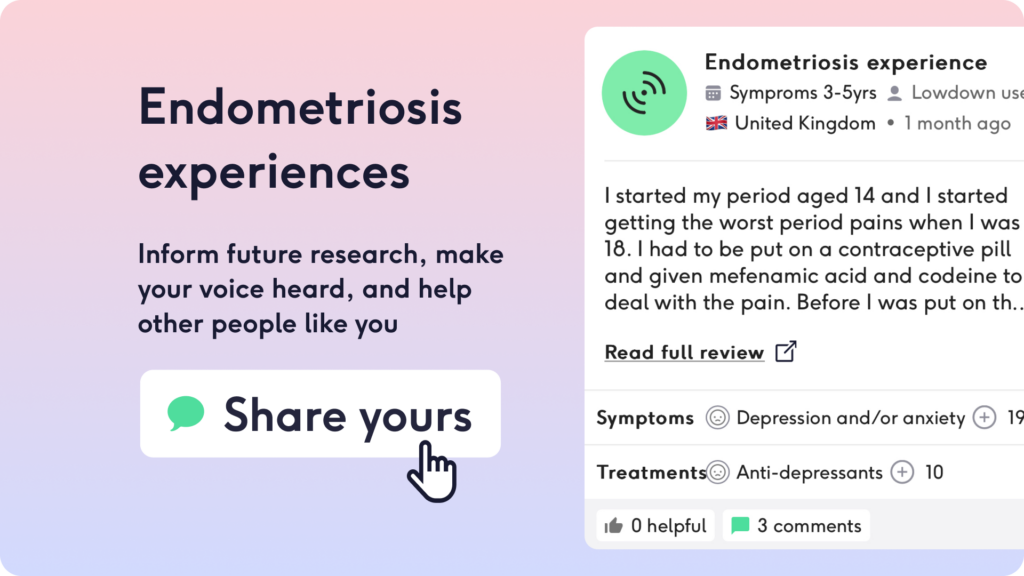
You can also go through our website, read our reviews or book in for individualised medical advice using our Speak to A Doctor service.
Endometriosis can be a life changing diagnosis. Please remember you are not alone and there is a community out there to support you. For further information see Endometriosis UK and if you’d love to understand more, watch our webinar event on endometriosis featuring a world specialists.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.