What is endometriosis?
What's the lowdown?
Endometriosis is a condition that can affect the whole body, with symptoms ranging from worse-than-average period pain and changes in your bowels to fatigue and brain fog.
In some people, endometriosis can affect their fertility.
✔️If you think this blog sounds informative, make sure to check out our newsletter for more:

What is endometriosis? How many people have it?
There are an estimated 190 million women and people assigned female at birth (AFAB) around the world affected by endometriosis (about 5-10% of those in their reproductive years).
The jury is still out on what causes endometriosis, but what we do know is that endometriosis causes clumps of cells to form outside of the womb that resemble the ones found inside the lining of the womb. These clumps bleed in the same way that the womb lining does, but the difference is the blood hasn’t got a place to escape from, so it stays behind, usually in the pelvis, and causes scarring, and more often than not, debilitating pain.
Over time, these clumps get bigger and can get stuck on other organs such as the bowel, bladder, ovaries and the surface of the womb.
Because diagnosis is difficult and often requires surgery, it can take many years to be diagnosed with endometriosis. A 2024 report by Endometriosis UK found that it takes on average 8 years and 10 months in England and Scotland to be diagnosed. Sadly, many people feel gaslighted by medical professionals who imply that their period pain is “normal”, which is also another reason why diagnosis can take so long.
What causes it?
There are a few theories on what causes endometriosis…
Retrograde Menstruation
For many years, the main theory, called “retrograde menstruation” attempted to explain that endometriosis starts because period blood travels up through the uterine (fallopian) tubes rather than out of the body through the cervix. It makes sense, but not for endometriosis, which can rarely be found in other places around the body such as the lungs and brain! Retrograde menstruation is thought to occur normally in up to 90% of women, so why doesn’t everyone develop endometriosis? Endometriosis is also found in newborns, prepubertal girls and men, so this simple explanation can’t be the full story.
Metaplasia
The coelomic (se-lo-mic) metaplasia theory says that endometriosis is caused when a trigger stimulates cells within the body to change from their normal function and structure, into cells similar to those found in the womb. It’s not a perfect theory though, because it doesn’t explain all the types of endometriosis such as that found in unborn foetuses.
Hormones and environmental toxins
This theory suggests that oestrogen causes growth of the endometriosis cells which are less reactive to progesterone, the hormone that normally keeps the lining of the womb in check. It is also thought that some environmental toxins mimic oestrogen and this causes further overgrowth of the endometriosis cells.
Oxidative stress and inflammation with apoptosis suppression
This theory says that DNA damage leads to an inflammatory response which encourages the overgrowth of endometriosis cells. Couple this with another theory that these cells don’t respond to the usual signals to breakdown when they are past their sell-by-date (known as apoptosis) and you have a potential recipe for endometriosis.
Immune dysfunction
It has been noted that autoimmune disorders are more common in women with endometriosis, so this has led to the theory that the immune system doesn’t function properly and this leads to endometriosis.
Genetics
There unfortunately isn’t one gene that is thought to be linked to endometriosis, but it does run in families, so genetics are thought to play a role in this condition too.
Stem cells
Stem cells are cells that normally turn into more mature cells in the body. They are the ultimate building block! They change into the cells needed after being triggered by chemical reactions in the body. A stem cell destined to become a stomach cell for example wouldn’t suddenly grow on your toe because it wouldn’t receive a signal to do that on your toe. There is a theory that stem cells lead to endometriosis cells because they don’t receive the correct signal to grow into the cell it is supposed to be. This explains why endometriosis can be found all over the body, and not just in the area near the womb.
The lowdown…It’s complicated
All these theories are interconnected, and all of them may be connected in some way. More research continues, so hopefully all of this knowledge will one day translate into better treatments and diagnostic methods.
What are the symptoms of endometriosis?
Periods
There are multiple symptoms of endometriosis, it isn’t just period pain. Periods can become heavy and bleeding could happen in between periods too, which looks like old or brown blood. Period pain can be felt in the anus, down the thighs and in the lower back. It can start in the days before a period begins and go on until the period finishes or even a few days after. Some people feel pain all the time, but it usually gets worse around the time of a period.
Body-function
Many women describe bloating, headaches and fatigue caused by endometriosis. As well as brain fog and difficulty making decisions which can make life feel even more stressful.
Urine and bowel symptoms
Going to the toilet to pass urine or stools can be painful and irritable bowel syndrome (IBS) is common. Sometimes there can be blood in the urine or the stools if the bladder or bowel is involved.
Sex
Sex can be painful and the pain is usually felt deep inside the pelvis.
Mental Health
Constant pain takes its toll. Women with endometriosis are more likely to suffer from depression and anxiety, as being in pain can make it hard to want to socialise with others who just don’t understand what you’re going through.
Everyday Life
It goes without saying that when faced with all of the above symptoms, daily life can feel tough. Endometriosis can even take a toll on your finances. Missed working days and the need to take on fewer hours to cope can all play a part, not to mention all the extra purchases like pain relief and supplements. Pain thresholds can be much higher in women with endometriosis, so they may need stronger pain relief than the average person for the same effect.
Stages of Endometriosis
When endometriosis is diagnosed, it’s categorised into 1 of 4 stages. This staging system was created by the American Society for Reproductive Medicine (ASRM).
|
Stage/Classification |
ASRM |
|
1 – minimal |
1-5 spots of endometriosis found, not deep |
|
2 – mild |
6-15 spots of endometriosis, starting to get deeper spots |
|
3 – moderate |
16-40 spots of endometriosis, many deep spots, small ovarian cysts, scarring |
|
4 – severe |
>40 spots of endometriosis, many deep spots, large ovarian cysts, severe scarring |
How can you tell if you have endometriosis?
Unfortunately, there isn’t a way you can know for sure if you have endometriosis until you have surgery (called a laparoscopy). This is done with a keyhole camera. Ultrasound scans can help, but unless the sonographer is highly experienced, it is unlikely to be seen on ultrasound unless it is very severe and obvious, so having a normal ultrasound scan does not rule out endometriosis.
MRI scans tend to be used once the keyhole surgery has identified endometriosis but it can be used before surgery to guide the next steps. MRI is used to determine where the endometriosis is and which organs are affected.
Does it cause any other health risks?
Endometriosis can cause issues with fertility. The more severe the stage of endometriosis, the more likely it will be harder to get pregnant. There are no absolutes though. The severity of endometriosis on appearance doesn’t always correlate to how hard or easy it is to get pregnant.
Talking to a healthcare professional about endometriosis
Keeping a diary of your periods and other symptoms is really helpful. Tracking how often you get symptoms, how severe they are, and how long they last for is exactly the kind of information you can share with your doctor during a consultation. It reduces the need for you to have to remember facts or dates and you can concentrate on getting your point across. Plus, it helps them to decide on the next steps, whether that’s monitoring your symptoms for longer, or referring you to another health care professional for further investigation.
When you are referred to a gynaecologist, be sure to ask them about their experience with endometriosis and what the next steps are should endometriosis be found (or not). Don’t be afraid to seek a second opinion if you’re not satisfied with the answers you get.
What can I do before going to my doctor?
It helps to discuss your symptoms so you can feel confident when seeing your GP. The Lowdown doctors can help you feel empowered to ask for a referral to a gynaecologist from your GP and can give you an idea of potential treatments.
The Lowdown doctors can also help you to decide on which contraception method is right for you should you be diagnosed with or have suspected endometriosis and choose to use contraception or discuss how to manage your symptoms.
What happens after you get diagnosed with endometriosis?
The main thing is to manage your symptoms in whatever way works for you. If you’re not trying for a baby, contraception can help to improve pain and slow disease progression. Unfortunately, it isn’t curable, but contraception and treatment to manage symptoms can massively help.
If you’re trying to conceive, then discuss a fertility referral with your doctor.
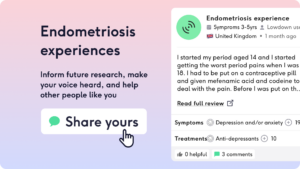
There are several support groups you can join, including the Endometriosis UK charity. You can also read endometriosis experiences and share your endometriosis experience on The Lowdown!
Got more questions about endometriosis? We’ve got you covered
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.