Endometriosis pain relief: what are my options?
What's the lowdown?
Endometriosis pain can range from dull aches to sharp stabs which can impact your daily life. Some people liken it to your body holding a protest every month, with endometriosis leading the way.
From over-the-counter medication to prescription powerhouses, there are many options to explore. And let’s not forget the non-pharmacological choices aka nonmedicinal choices – think cosy heat packs and mindfulness tricks. These can work wonders if medicines aren’t your thing or they aren’t helping to ease your symptoms.
When your body starts sending out those SOS signals, it’s time to get some help. Whether the pain’s throwing a full-blown party, or new symptoms decide to gatecrash, don’t hesitate to reach out. You know your body the best, and you’ll know when you need help.
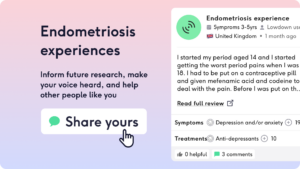
Ready to swap stories and tips with fellow endo warriors? Look no further than The Lowdown. You can dive into the real-life experiences shared by people who’ve been there, done that, and are going through exactly what you’re going through.
And why not share your own journey? Your story could be just the lifeline someone else needs.
So, you’ve heard about endometriosis and those pains it brings along? Let’s dive into the world of endometriosis pain relief – because nobody should have to grin and bear it.
What causes my endometriosis pain?
Have you ever felt like your body’s staging a protest every month? If you have endometriosis, this is a reality that many people face. This condition throws endometrial-like tissue to places where it shouldn’t be, causing inflammation and, you guessed it, pain. From annoying dull aches to sharp stabs, endometriosis pain is no joke. But we’re here to help you understand this pain and find ways to relieve it.
Endometriosis is a chronic condition where tissue similar to the lining of the uterus grows outside the uterus [1]. During menstruation, this tissue behaves similarly to the uterine lining, breaking down and bleeding as it responds to hormonal changes. However, unlike the lining of the uterus, this blood and tissue have no way to exit the body, causing inflammation, pain, and the formation of scar tissue. This can lead to a variety of symptoms, including pelvic pain, painful periods, pain during intercourse, and infertility.
Understanding the source of endometriosis pain is crucial for dealing with and managing this pain. While the exact cause of endometriosis pain is not fully understood, it is thought to be primarily due to inflammation caused by the presence of endometrial-like tissue outside the uterus [2]. This inflammation can irritate surrounding tissues and nerves, leading to pain which is felt in many different ways.
For some people, common triggers of endometriosis pain include:
- Hormonal changes, especially around menstruation
- Certain foods, like foods high in sugar or caffeine
- Feeling stressed
- Lack of sleep
- Physical exertion
How can I help my pain?
Immediate and long-term relief can help with endometriosis pain.
Immediate relief includes:
- Pain relief: Over-the-counter options like ibuprofen and paracetamol or prescribed medication to provide temporary relief
- Heat therapy: Heating pads or warm baths can help to soothe muscle cramps and pain
- TENS machines like the Myoovi.
Long-term relief includes:
- Hormonal treatments that can help to manage pain by regulating or stopping menstruation
- Lifestyle changes like regular exercise, a balanced diet and stress management techniques like yoga or meditation
- Surgical treatments
So, what’s in your pain relief toolkit? From over-the-counter medication to prescription powerhouses, there are many options to explore. No one should have to live in constant pain. When it comes to pain relief, it’s all about finding what floats your boat and what is suitable for you and your lifestyle.
Over-the-counter pain relief such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or mefenamic acid can be effective in reducing endometriosis pain. These work by reducing inflammation which can help to relieve discomfort. If you do take any NSAIDs, make sure to take them with a meal, snack or a drink of milk. This can make them less likely to upset your stomach.
If these don’t work, make sure to speak to your doctor. They might prescribe stronger pain medications or hormonal therapies to help manage symptoms. Hormonal therapies are a whole other area to explore which are a mainstay of treatment for endo pain so be sure to check out our blog.
Non-pharmacological approaches can also play a huge role in helping to manage endometriosis pain. Heat therapy, such as using a heating pad or warm bath, can help relax your muscles and reduce any cramping you might have. Additionally, techniques such as acupuncture, yoga, and meditation may help reduce stress and improve overall well-being, which can in turn help manage pain [4].
Let’s chat about TENS machines (Transcutaneous Electrical Nerve Stimulator) – an alternative to traditional pain relief. They work by attaching to the skin via electrodes and sending electrical impulses into the body. These impulses don’t hurt, instead they feel ticklish. So, how do they work their magic? Well, scientists still aren’t completely sure but think they either work by blocking pain messages as they travel through your nerves, or they help your body to produce their own natural pain relief called endorphins.
And here’s the cherry on top – some TENS machines like the Myoovi are so handy; you can just stick them to your skin. We’ve put together a handy guide of Myoovi reviews so you can see if it’ll work for you. And finally there is the magic of the pelvic health physiotherapist who can be absolutely game changing for endo pain, and unfortunately not many people know about them!
Thankfully, this reviewer found one and recommends them to everyone…
“One of my best pieces of advice would be to see a pelvic floor physio.”
Does endometriosis pain ever go away?
For some people, endometriosis pain may lessen with age or after the menopause. However, many people need ongoing management to cope with the symptoms. Endometriosis management aims to help you reduce pain and improve quality of life, rather than curing it.
When should I speak to a doctor?
When your body starts sending out those SOS signals, it’s time to speak to your doctor. Whether the pain’s throwing a full-blown party or new symptoms decide to gatecrash, don’t hesitate to reach out. Your doctor has the expertise to guide you through the maze of treatment options and get you back to feeling like yourself again. Sometimes it can be daunting to speak to them, but you can use our handy guide here. You can book an appointment with one of our women’s health doctors to help you get to the bottom of a problem or help you to put a pain management plan into action. After all, everyone deserves to be listened to!
While the occasional pelvic pain can be common and may not necessarily mean there’s something serious happening, if you have persistent or severe pain that isn’t settling with paracetamol and ibuprofen or is stopping you from doing your day to day tasks, this shouldn’t be ignored.
If you have symptoms like severe pelvic pain, pain during intercourse, heavy or irregular periods, or difficulty getting pregnant, it’s so important to seek medical advice. Your doctor can help you manage your symptoms and if needed, help to develop an appropriate treatment plan.
Are there any exciting developments on the horizon for endometriosis?
Research into endometriosis is ongoing, with new treatments and management strategies continually being explored. Recent studies suggest that genetic factors can play a role in the condition, which can pave the way for potential new therapies. [5]
What have the community got to say?
Ready to swap stories and tips with fellow endo warriors? You’re at the right place. Look no further than The Lowdown.
People have shared experiences like:
“Hot water bottles were really good. Didn’t take the pain away but the heat helped my body to loosen up a bit”
You can dive into real-life experiences shared by people who’ve been there, done that, and lived with endometriosis. Why not share your own journey? Your story could be just the lifeline someone else needs.
The Lowdown provides a platform for individuals to share their experiences with endometriosis, including their struggles, triumphs, and tips for managing symptoms including endometriosis pain. By sharing your own experiences and learning from others, you can gain valuable insight, support and become a community with other people who know and understand what you’re going through.
Whether you’re looking for advice on managing pain, coping with emotional challenges, or navigating treatment options, The Lowdown’s endometriosis community is here to offer support and solidarity. Join the conversation, share your story, and connect with others who are on this journey with you.
Living with endometriosis pain isn’t always a walk in the park, but armed with the right tools and support, you can conquer those tough days and enjoy your life. Having endometriosis doesn’t mean you can’t live well! Keep learning, keep connecting, and remember, you’re never alone on this journey.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.

