What is ‘endo belly’? Endometriosis and bloating
Does Endometriosis cause bloating?
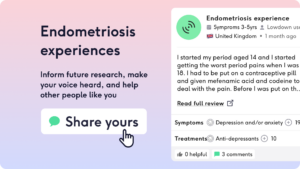
Endometriosis is a common women’s health condition affecting around 1 in 10 women. If you’re an endo sufferer, you know that there is a wide range of symptoms including pain, diarrhoea, fatigue, urinary symptoms…..and also bloating. Here we delve into endometriosis bloating, helped by descriptions from our Lowdown community.
What is endo belly?
Endo belly is bloating or swelling of your abdomen usually due to gas, which usually happens just before and during your period. The endometriosis bloating can feel like a tight pain and cause a lot of discomfort. It is defined medically as “cyclical bloating of the abdomen”.[1]
“…bloating that worsens pre-menstrually and menstrually”
Is endo belly or bloating a common symptom of endometriosis?
Endo belly or bloating is a very common symptom. In fact, bloating is really common in anyone who has a period. However, if you don’t have endometriosis, bloating will affect around 2/3rds (64%) of people, compared to almost all (96%) of people who have endometriosis. Endo belly is known to be more extreme than usual period related bloating.[2]
What causes bloating or endo belly?
Endometriosis causes deposits of tissue similar to the womb lining to grow outside of the womb, such as on the pelvic wall, ovaries or intestines. These deposits thicken and bleed throughout your menstrual cycle causing inflammation in your pelvis and abdomen. An imbalance of the gut microbiome is thought to worsen this inflammation. Over time (and we know endometriosis takes a LONG time to diagnose), this increased inflammation causes bloating, abdominal and pelvic pain and bowel symptoms.[1]
What’s the difference between endo belly and IBS?
Endo belly and IBS can have similar overlapping features of bloating and bowel changes, meaning that patients can get diagnosed incorrectly with IBS when the problem is actually endometriosis.
The key differences are the triggers and patterns of the bloating. Endo belly is almost always associated with periods and the menstrual cycle, whereas IBS bloating happens after eating certain foods or due to stress and doesn’t follow a monthly pattern.[3]
Is endo belly hard or soft?
Everyone experiences endo belly differently, but usually it will feel tight or hard. However, if you have soft bloating, this doesn’t mean it isn’t caused by endometriosis, especially if you have other symptoms such as very painful periods.
What are the gut related symptoms of endometriosis?
Endometriosis has been described as a “systemic” disease which means it is widespread and affects many different organs.[4] The intestine can be involved as endometrial deposits can be found both on the surface of, or penetrating into the gut wall.[5] The gut related symptoms of endometriosis include:
- Abdominal pain
- Nausea and vomiting
- Pain on opening the bowels
- Constipation OR diarrhoea
- Bleeding from the back passage
- A sensation of not fully emptying the bowels called tenesmus
When is it not normal bloating? When should I see a doctor?
While bloating is common in endometriosis, it can also be found in other conditions. Bloating can be a normal part of your menstrual cycle, or a PMS symptom but may be a symptom of other gut conditions such as coeliac disease, inflammatory bowel disease and not forgetting pregnancy!
If you have severe, tight bloating every month, especially if this is alongside bowel symptoms, bleeding from the bowels, weight loss, vomiting after eating or a change to your periods, then please see a doctor.
How to treat endo belly?
To treat endo belly, you should firstly make sure you have a formal diagnosis of endometriosis and get treated for the condition. If you’re not sure where to start, ask one of the Lowdown doctors.
Traditional treatment of endometriosis includes:
- Hormonal therapy including with contraceptives
- Medications to block the oestrogen which drives endometriosis
- Surgery including laparoscopy or hysterectomy
Endometriosis bloating relief
We know that holistic treatment is very powerful to treat endo belly symptoms including:
- Reducing stress. The amount of stress you are under correlates to how severe your endometriosis symptoms are.[6]
- Pelvic health physiotherapy. Endometriosis pain can cause your pelvic floor and lower abdominal muscles to tense up. Relaxing these muscles can help to ease your pain.[7]
- Sleeping well, as good sleep reduces stress….see the first bullet point.
- Regular exercise has been reported to improve endometriosis pain by patients but the research is yet to catch up.[8] Movements and exercise can also help move the air around your abdomen to improve the bloating in endo belly.
- Dietary changes. Although high quality research is lacking in how diet affects endometriosis symptoms, many people believe an anti-inflammatory diet can help. Avoiding foods which cause bloating such as beans, sprouts and dairy could reduce endo belly – why not try tracking what you eat and see if you notice a difference?
If you found this useful, please leave your own endometriosis experience so we can help plug the gaps in research and help others at The Lowdown.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.