
Everything you need to know about PCOS | FAQs
What is PCOS?
PCOS stands for polycystic ovary syndrome. It is common, affecting around 10% of women and can be described as a hormonal, metabolic or endocrine condition. PCOS is a collection of signs and symptoms which can include: irregular or absent periods, high levels of testosterone in the bloodstream (which can cause acne or unwanted hair growth) or a typical appearance of the ovaries on an ultrasound scan. Women experience PCOS and the symptoms in many different ways, which you can see from our shared experiences.
PCOS can have an impact on many aspects of your health, which are important to be aware of so you can manage them. These include your cholesterol level, diabetes risk, fertility and risk of womb cancer. This sounds scary, but knowledge is power, so read more to learn about how to manage these risks.
What causes PCOS?
We don’t fully understand what causes PCOS yet, but we do have some clues.
There is a genetic link where some women inherit a higher risk of developing PCOS. However, many other factors also play a role as to why these women go on to develop PCOS such as diet, exercise and other lifestyle or environmental factors.
Hormones are key in PCOS – with testosterone and insulin being major players. Testosterone levels are usually higher in those with PCOS, which can cause some of the symptoms.
People with PCOS may be “insulin resistant” which means their body doesn’t react as well to the hormone insulin. Insulin is the hormone which helps our body store and use sugar from food. Insulin resistance seems to affect the functioning of the ovaries and contributes to the hormonal imbalance in PCOS.
We all agree that there isn’t enough research into PCOS – how do we not even know what causes a condition that affects 10% of women!
How is PCOS diagnosed?
Currently, to diagnose PCOS, doctors use the “Rotterdam criteria”. This is a triad of signs or symptoms and you have to meet 2 out of the 3 to be diagnosed.
These are:
1 . Irregular or absent periods
Medical definition – less than 8 periods per year or a cycle length of less than 21 or more than 35 days OR no period for over 90 days
2. High levels of androgens
Medical definition – a higher than normal level of testosterone on blood tests OR unwanted hair growth, acne or hair loss
3. Appearance of polycystic ovaries on an ultrasound
Medical definition – more than 20 follicles (small fluid filled sacs) seen on at least one ovary OR an ovary that is more than 10ml in size
Recent guidelines suggest that a blood test called AMH (anti-mullerian hormone) could be used instead of an ultrasound scan which might help speed up diagnosis. It’s important to know that an ultrasound and AMH level can’t be used for diagnosis of PCOS within 8 years of you starting your period.
What are ovarian cysts v ovarian follicles?
We have no idea why it’s called polycystic ovary syndrome because they’re not actually cysts that are found on the ovaries, they are follicles. Follicles are small fluid filled sacs on the ovary which contain immature eggs. In PCOS, these follicles don’t mature and release their egg so they accumulate on the ovary and can be seen on ultrasound.
Ovarian cysts, however, are fluid filled sacs that don’t contain an immature egg and are over 3cm in size. Ovarian cysts are really common and don’t necessarily mean you have PCOS.
Can you get pregnant with PCOS?
Yes, you can get pregnant with PCOS! 60% of those with PCOS will have no problems getting pregnant. Even for those couples who find it more difficult to conceive, fertility treatment is usually successful. If you have PCOS or suspect you do, getting early advice can really make a difference. Our specialist fertility nurse can help you get started to optimise your fertility and using Ovusense (highly recommended by our community) identifies where in your cycle you need support.

Can you develop PCOS in later life?
PCOS symptoms can appear at any point in your reproductive life. However, it’s most common to have symptoms from your late teens into your 20s. Many people discover they have PCOS at the point of trying to get pregnant, or if they start to gain weight. However, the advice and treatments are still the same, whatever age you are. We know that the symptoms caused by high levels of androgens in PCOS can persist after menopause, so may continue well into later life in some people.
What is the difference between PCO and PCOS?
PCO is when your ovaries have the appearance of polycystic ovaries on ultrasound but you don’t have any other symptoms of PCOS. Medics and scientists actually use the abbreviation PCOM (standing for polycystic ovary morphology) on ultrasound scan. PCOS is the ultrasound changes combined with the symptoms needed for diagnosis (see above…). We don’t know why some people have PCO but no symptoms, and others do – but it’s likely a combination of genetics, lifestyle and environmental factors that contribute.
PCOS symptom FAQs
What are the first signs of PCOS?
The first signs of PCOS can be different for each individual. The most common ones are likely to be:
- A change in your cycle, often becoming more irregular, usually with more than 35 days between each period
- Worsening acne that might not be easily treated
- Hair growth in unwanted areas like on the chin, face or around the nipples, on the chest or the back
- Thinning of your hair all over the head
- Weight gain despite no change in diet or exercise
- Struggling to get pregnant.
However, everyone is individual, so symptoms can start at different times and you may experience a combination of the above. Please leave a review about your PCOS symptoms to help others. In some cases there may be other causes for these symptoms and if you’re worried, make sure you speak to your healthcare professional.
What are the main symptoms of PCOS?
The main symptoms of PCOS are:
- Irregular periods or even none at all
- Weight changes including rapid weight gain and struggling to lose weight
- Acne or oily skin
- Unwanted hair growth on the face or body, which is called hirsutism
- Loss of hair or thinning of the hair on your head
- Mood changes including depression and anxiety
- Difficulty getting pregnant and miscarriage
However, this is not an exhaustive list, there are many other signs and symptoms that are caused by PCOS which research and our community describe.
Some of the other symptoms and other factors that may impact on your health include:
- Disordered eating
- Insulin resistance
- Snoring (from a condition called obstructive sleep apnoea)
- Sexual problems
- An increased risk of high cholesterol, high blood pressure, type 2 diabetes and gestational diabetes
- Overgrowth of the womb lining which over many years may develop into cancer
This may be a lot to read and feel very overwhelming. But don’t worry, the first step is a diagnosis, then with good management, you are often able to control many of these symptoms with a collection of monitoring, lifestyle changes and sometimes medications.
Is PCOS painful?
Some people say that polycystic ovaries cannot cause pain, but every person will experience PCOS symptoms in different ways, and at The Lowdown we believe in listening to and validating your experience. Many of our community say that PCOS can be painful.
Pain felt in PCOS could be due to a multitude of reasons; ovulation pain, heavy periods, bloating or cystic acne. It is important, however, to not attribute all pain to your diagnosis of PCOS, and if something does not feel right with your body, get it checked out by a healthcare professional.
Can you have PCOS and endometriosis?
Yes, you can have both PCOS and endometriosis. Both are separate conditions, and both affect around 10% of the female population so there is likely to be many people who suffer from them both. And of course, this includes some of The Lowdown community. If you want to hear from more people who have suffered from both conditions, search for endometriosis through our PCOS experiences.
PCOS treatment FAQs
What treatments are there for PCOS?
There are many different treatments for PCOS, some which focus on specific symptoms, and others which treat your overall health.
Often the most successful treatments are lifestyle changes. These can be hard to stick to, but by making small changes in lots of areas, they can add up to a huge difference. Concentrate on exercise, moving your body and using your muscles and focus on healthy diet changes that you can stick to. These will help your PCOS symptoms, any mood or anxiety symptoms and improve your overall health and wellbeing.
However, the treatments below can help with more specific symptoms.
- Irregular periods can be treated with hormones and contraceptives or with supplements containing inositol such as MyOva.
- Acne treatments can be bought from pharmacies and creams or antibiotics can be prescribed from your GP. The combined pill can help, but if you can’t use it, then specialist doctors can prescribe strong drugs called spironolactone or Roaccutane (also called isotretinoin).
- Hair growth is frustrating but can, again, be helped by hormonal contraceptives (read more about the best pill for hair growth) or by hair removal methods like waxing, plucking, creams or laser.
- Fertility treatment is available if you are trying to conceive from specialists. You can learn more about PCOS and fertility here.
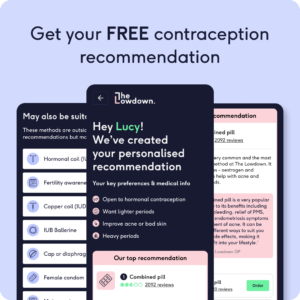
What contraception is best for PCOS?
The best contraception for PCOS depends on the symptoms you are treating. The combined pill is very good at treating acne and irregular periods. Pill brands such as Yasmin, Eloine or Dianette which contain a progestogen that reduce the effect of androgens associated with PCOS may be better than standard combined pills.
Other contraceptives can be excellent at controlling heavy, irregular bleeds and also help protect the womb lining from overgrowing, which is a risk with PCOS if you have irregular periods. These include the hormonal coil, progestogen only pill, implant and injection.
Is there a diet that’s best for PCOS?
No, there is no diet that is best for PCOS. Some healthcare professionals will advocate a keto or low carb diet, but there is no evidence that this is better than any other type of diet. The best diet for PCOS, is an overall healthy one, that you can stick to day to day without developing disordered eating and that keeps you feeling good about yourself. Aim to make healthier choices, include plenty of fruit, vegetables and fibre and just keep an eye on portion size. If you’re aiming to lose weight, do this slowly and steadily, and if you need more support, speak to a dietitian or nutritionist who has expertise in women’s health or PCOS. If you’ve found a particular approach helpful – please share your experience to help others.
How can I lose weight if I have PCOS?
Weight loss in PCOS is complex and can be difficult – but it isn’t impossible. However, the approach from our Lowdown doctors may shock you. They advise you to stop looking at the scales and measuring weight. Yes, we know that PCOS symptoms and your overall health improve with weight loss, but we also know that the pressure to lose weight and weight stigma affect your mental health and risk disordered eating. Instead focus on fitness, move your body and use your muscles (really important in PCOS as more muscles helps your metabolism). Concentrate on a healthy diet and normal portion control. By having an overall health approach, rather than focussing on weight, you will often find that weight loss follows.
However, if you want specific help, speaking to a dietician or health coach can help with advice and to set goals.
Metformin is a medication which can be offered to women who have PCOS as it can manage symptoms, improve insulin resistance and can help with weight loss.
Newer injectable medications such as ozempic may be available if you have a high BMI and other health problems such as high blood pressure or type 2 diabetes, which are more common in people with PCOS.
Remember, with the right information, support and motivation you CAN lose weight with PCOS, but don’t be disheartened if you need to try a few different lifestyle changes to see those scales move, go off how you FEEL. Check out our user experiences to see how other women have managed, or leave your own to help others.
Can you cure PCOS permanently?
Unfortunately, you can’t cure PCOS permanently. The high levels of androgens associated with PCOS which can cause many of the symptoms persist after menopause. However, you can manage the symptoms.
It’s really important to understand the long term implications of PCOS to your health, especially as the condition won’t go away.
If you have PCOS, you are at a higher risk of developing high blood pressure, high cholesterol and type 2 diabetes. We don’t want to panic or upset anyone but you should know this so you can take steps to look after your health and prevent these. You need to make sure you attend regular monitoring and health checks as you get older to pick up any problems early. Finally, bleeding is very important. Unless you are on hormonal contraception, you have to bleed 4 times a year if you have PCOS. If you don’t, you are at risk of your womb lining overgrowing which over many years can become cancerous. Your doctor can prescribe hormonal medication 4 times a year to induce a bleed if you do not want hormonal contraception. And finally, if your bleeds suddenly change and become much heavier – speak to a doctor, because this can be a sign of overgrowth of the womb lining and if you have PCOS, you should be offered further investigation.
Again, we don’t mean to scare you. PCOS can’t be cured but can be managed, as long as you have the right information and education to empower you!
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.


