Can the contraceptive pill cause headaches and migraines?
In this article
What's the lowdown?
With or without the pill, women are naturally more prone to headaches and migraines
Both pill types can make headaches and migraines worse, better or unchanged
If you have migraines with aura the risks of using combined methods outweigh the benefits
If you have headaches or migraines without aura on the combined pill related to your pill-free break, continuous combined pill taking could be the answer
Take a look at our The Lowdown reviews to see headache and migraine occurrences on different contraceptives as they can be super variable from person to person
There is help out there so please see your GP if you suffer with headaches or migraines – they are likely to ask you to keep a headache diary to track your symptoms as a first step towards diagnosis and treatment
Headaches, migraines and the contraceptive pill…
A common side effect of the contraceptive pill can be headaches, with up to one third of women experiencing migraines.
Migraines are a type of headache disorder which affects around 6 million people in the UK every day, with an estimated 5-25% being women. In fact from puberty onwards, women are much more prone to migraines than men. This typically continues apart from improvements that can be seen during pregnancy and after the menopause (well there’s got to be some silver linings!).
This might provide a clue to the connection that has been identified between hormonal fluctuations and migraine – which is exactly what we’re going to explore here.
Read on for a deep dive into the symptoms, treatments and contraceptive options for migraines or headaches.
First things first… headache or migraine – what’s the difference?
Often following an evening of pinot grigio comes the banging head and throbbing temples. But what exactly defines a headache? There are many types of headache, with the most common being tension headaches. Symptoms wise, this can feel like a constant dull ache, which may include neck pain and a feeling of pressure behind the eyes. Real nice.
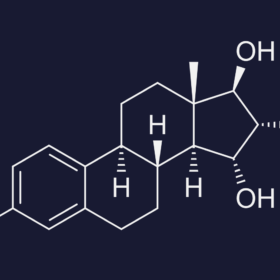
However, as this is The Lowdown we’re here to focus on headaches, migraines and the pill. Hormonal headaches can be caused by fluctuations in hormones such as oestrogen, throughout the menstrual cycle. If you track three or more cycles and notice these headaches occuring in a regular pattern throughout certain times of the month, chances are it could be triggered by hormonal fluctuations in your menstrual cycle.
The NHS defines migraine headaches as a ‘moderate or severe headache felt as a throbbing pain on one side of the head’, although there can be variations on this. Typical associated symptoms include nausea and light and sound sensitivity. You can also think of the throbbing headache as being a symptom of migraine, as the migraine itself can incorporate lots of other things including vision changes, dizziness or nausea. In fact, you might not even experience a headache at all.
What symptoms can migraines cause?
There are a couple of classifications of migraines; migraine with aura and guess what – migraine without aura. Aura is a term used to describe any sort of neurological disturbance, which can appear before the headache or other symptoms of a migraine. Around 10-30% of migraine sufferers experience these symptoms.
Aura is usually visual, including flashing lights, coloured spots or zig zags in the field of vision. This can be extremely frightening the first time it happens, but typically subside within an hour. Other neurological symptoms such as weakness on one side, dizziness or vertigo can happen. It’s important to remember that if you have neurological symptoms like weakness on one side, difficulty speaking or losing your vision for the first time, don’t just assume this is a migraine, get help from a doctor quickly by calling 999 to rule out any other cause first.
Why do I get migraines anyway?
There are so many alleged triggers for migraines, from chocolate to the weather! Changes in female sex hormones such as oestrogen and progestrone are also linked to the onset of migraines. Sufferers may have noticed that migraine symptoms seem to be triggered at the same time each month, coinciding with different points of the menstrual cycle. Research suggests that this could be due to the drop in oestrogen just before your period and the release of prostaglandins (which cause uterine contractions) at this time. Oh, and naturally, if you then start taking a form of contraception such as the pill, migraine symptoms might change or worsen as those hormones are affected.
Diagnosing a migraine headache
If only it was as easy as a blood test…(said no one, ever).
To diagnose migraines, your GP needs to build up a record of frequency, symptoms and patterns of your headaches. During your first appointment, a physical examination may also take place, including blood pressure, vision and coordination tests. Depending on severity and complexity, diagnosis may also involve a referral to a specialist neurologist.
Headache diaries to track your menstrual cycle
You might want to think about noting down your headaches alongside any other symptoms, each time you get them. This can really help clinicians to build a picture of how your headaches or migraines present, and ensure they can give you the best advice on treatment options. There’s a whole host of useful information that you can begin to track including
- Time and date
- Length of attack
- What triggered it
- Other symptoms like nausea, vomiting, light sensitivity or neurological symptoms
- Painkillers taken (which ones, how much and when)
- What you were able to do while you had the headache (aka could you do nothing other than lie in a dark room, or were you able to do the weekly big shop)
It would also be handy to note down where in your menstrual cycle the headache or migraine was, as this can help see whether there is a hormonal link.
The pill, migraines and headaches: let’s discuss…
Can the contraceptive pill cause headaches and migraines?
Yes, the combined pill can cause headaches and migraines. If you’ve ever read the back of the pill packet, headaches are listed as a side effect, and although in many cases they tend to lessen over time, studies suggest headaches can be one of the leading reasons for pill discontinuation.
Some users may find that their headaches worsen while using the combined pill, especially during the pill break. This can be caused by the drop in oestrogen when you have a break.
Women who have migraines without aura, are able to try the combined pill with caution. Some people will find their migraines get worse or more frequent on the combined pill – and if this is you, you should stop it and choose a different option. However, others, especially if you use the pill back to back, might notice their migraines improve or become less frequent.
Migraines and the pill – is it safe to take?
If you suffer from migraines with aura, then the combined pill, (which contains oestrogen and progestogen) is unsuitable, due to a very small increased risk of ischaemic stroke. This risk was identified through studies in the 1970s, when much higher doses of oestrogen were used in pill formulations.
Although there can be differences of opinion in the risk versus benefits – it is important to discuss with your GP if you wish to be prescribed a pill and suffer from migraines. Your doctor will not prescribe the combined pill if you experience aura symptoms with migraines. In some cases it may be fine to be prescribed the combined pill if you experience migraines without aura, but you should go back to your healthcare professional if your migraines worsen and discuss a different option.
Of our Lowdown community, 16% experienced headaches, 7% experienced migraines without aura, and 3% migraines with aura on the combined pill (data taken October 2024).
Can the mini pill give me headaches or migraines?
The mini pill, injection, implant and hormonal coil are safe for use for those with migraines both with and without auras, however headaches are still a recognised side effect of progestogen-only contraception.
What about headaches with the implant and injection?
The injection and implant forms of contraception do not contain oestrogen and only contain progestogen so are safe to take if you have experienced migraine with (or without) aura.
15% of Lowdown reviewers experienced headaches on the mini pill, compared to 7% of reviewers reporting migraines – so no real difference at all when compared to the combined pill. The figures are higher for the injection (25% – headaches / 11% – migraines), which is unusual as the injection is ofetn used to prevent menstrual migraines. And the implant (15% – headaches / 7% – migraines) is again similar to the pills. (Data taken October 2024)
Headache and migraine friendly contraceptive options
There are a few options which showed much lower headache and migraine prevalence among The Lowdown community. It’s important to remember though, that lot’s of these users will have headaches and migraines that actually aren’t related to their contraceptive choice at all!
Hormonal coil: 9% headache, 5% migraine
Copper coil: 8% headache, 4% migraine
Natural cycles: 4% headache, 21% migraine
Male condom: 2% headache, 0% migraine
Not to keep banging on about it, but side effects vary hugely and you might find you’re the total opposite to the numbers above. (Oh, and if you are – please let us know by submitting a review as it’s super insightful).
Continuous pill taking – no more migraines!
Normally with the combined pill, there’s 21 days of taking the pill, followed by a 7 day break. However, taking your pill non-stop could be the answer to keeping those migraines at bay. Skipping the 7 pill free days, and maintaining oestrogen levels has been shown to be effective in studies (wahoo!) as well as potentially helping with other PMS (pre-menstrual syndrome) symptoms. This could be something to discuss with your GP if you are experiencing headaches or migraines during your pill-free breaks.
I’m getting migraines / headaches – help!
Whether or not you’re taking the pill, over the counter painkillers to manage the onset of headaches or migraine could be the answer. However, if this has not been effective your GP will be able to look at other treatments including anti-sickness drugs or medicines called triptans (that specifically target migraines).
There are other recommendations that could keep life more pain-free:
- Food glorious food: maintaining your blood sugar levels by eating regular snacks and meals – as skipping meals can trigger migraines
- Catching some zzzz’s: make sure you have a consistent night time routine and enough sleep each night
- Calm and collected: stress is another trigger, so it might be useful to develop an exercise routine or mindfulness strategies such as yoga.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.