Pelvic organ prolapse symptoms, causes & treatments
In this article
What's the lowdown?
Pelvic organ prolapse is when organs in the pelvis move and can drop lower than where they would usually be
The pelvis is held together by pelvic floor muscles and weakening of these muscles can lead to prolapses
Prolapses can be mild to severe and do not always cause symptoms
Depending on the severity and type of prolapse, there are different treatment options available to you
Pelvic organ prolapse is common, and you should not be embarrassed about seeing a doctor about your symptoms
Treatment can improve your quality of life
What is pelvic organ prolapse?
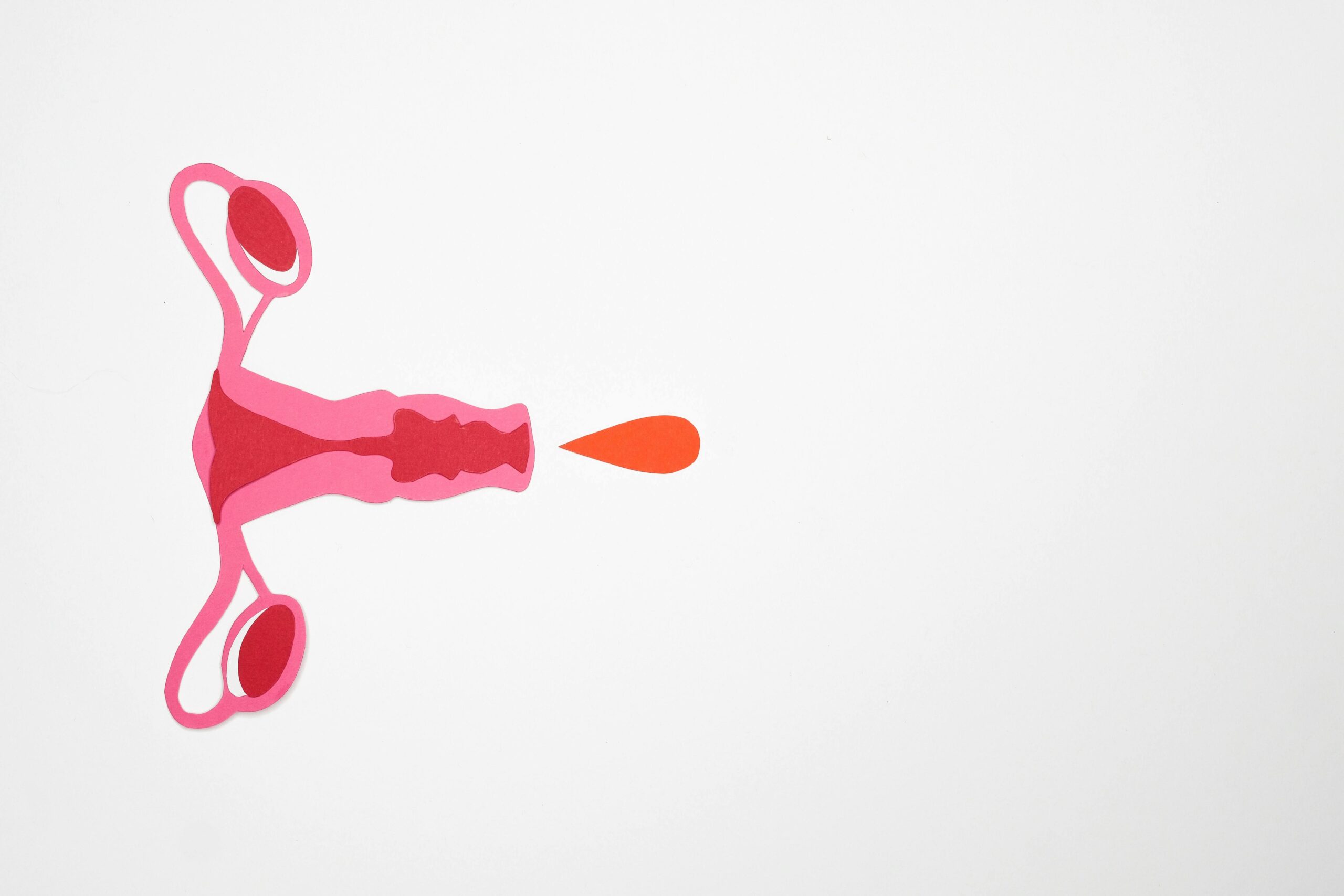
Pelvic organ prolapse describes the movement of one or more of the organs found in the pelvis out of its original position down into the vagina(1).
The organs in our pelvis are held together by our pelvic floor (made up of muscles and ligaments). When these supportive muscles and ligaments become overstretched, they weaken causing the organs to move from their natural position into the vagina and form a bulge. Depending on the severity of prolapse, the bulge can even protrude from the vagina(1).
The organs that can move include the bowel, bladder, womb or the top of the vagina. Pelvic organ prolapse is not a natural part of ageing but is very common and can affect 25% of women in their 40s and 33% of women in their 60s. Over 50% of women in their 80s have some form of pelvic organ prolapse(2).
But, while pelvic organ prolapse is not life-threatening, it can definitely cause symptoms like discomfort and pain. Sometimes pelvic organ prolapse can prevent you from doing things you love and enjoy, affecting your quality of life(1).
Pelvic organ prolapse symptoms
Not all prolapses can lead to symptoms, and you might only find out you have a prolapse on a routine pelvic exam or during cervical screening. Mild pelvic organ prolapse may not cause any symptoms and do not necessarily need treatment.
Symptoms of pelvic organ prolapse include(3):
- A heavy feeling around your tummy and vagina
- A dragging sensation inside your vagina
- Noticing a lump inside or outside of your vagina
- Uncomfortable sex
- Urinary symptoms like increased need to urinate, not being able to empty your bladder fully or leakage or incontinence while coughing, sneezing or exercising
Pelvic organ prolapse types
The organ prolapsing into the vagina determines the type of pelvic organ prolapse. It is common to have more than one organ move and drop at the same time. The stage of the prolapse depends on how far the organ is coming down or out of the vagina. The treatment for each type and stage of prolapse differs(4).
Anterior wall prolapse
This type of prolapse describes the bulging of the bladder and/or the urethra (the tube that guides the urine out of your bladder into the body) into the front of the vaginal wall. Another technical medical name for this is the cystocele (only involving the bladder) or cystourethrocele (involving both bladder and urethra).
Posterior vaginal wall prolapse
This prolapse occurs when the rectum protrudes into the back of the vaginal wall, also referred to as a rectocele. Sometimes the small bowel might follow as well and in this case, it is called an enterocele.
Uterine prolapse
As the name might suggest, this type of prolapse involves the uterus (also called the womb) moving down into the vagina, at times even coming out of the vagina completely. This extreme form of prolapse is referred to as procidentia.
Vault prolapse
When the upper part of the vagina sags down it is known as the vault prolapse. This is more common in women who have had their uterus removed (hysterectomy).
What causes pelvic organ prolapse?
Pelvic organ prolapse develops due to the weakening of the pelvic floor, which means the organs aren’t fully supported and so drop or bulge downwards. Certain events and conditions can make prolapse more likely to happen, or worsen the prolapse. These include(3):
- Pregnancy
- Childbirth
- Menopause
- Being overweight
- Regular constipation
- Heavy lifting
How is pelvic organ prolapse diagnosed?
The most common way of diagnosing pelvic organ prolapse is by an internal pelvic examination with a speculum. Clinicians are able to identify which organs are pushing down while they examine you. The stage of a prolapse depends on how much the bulge is coming out of the vagina. Grade 1 is mild where the prolapse hasn’t reached the opening of the vagina, a grade 2 prolapse is where the bulge of the prolapse just reaches the entrance of the vagina. Usually, mild prolapses are unnoticeable and do not require treatment(1). A grade 3 prolapse has moved down out of the vagina. Grade 4 is the most severe type of prolapse where the organ has come as far down as it possibly can out of the vagina.
Pelvic organ prolapse treatment
The treatment you will be offered depends on the type and severity of the pelvic organ prolapse. Your doctor will also tailor your treatment to your age, overall health and whether you have completed your family. These are some of the treatment options you may be offered(4).
Pelvic organ prolapse lifestyle changes
Small and simple changes to your lifestyle or daily habit can improve your prolapse:
- Weight loss
- Smoking cessation
- Preventing constipation
- Avoiding lifting heavy objects or weights
- Avoiding exercise that can impact your pelvic floor (running/trampolining)
Pelvic organ prolapse exercises
Strengthening your pelvic floor is also a great way to improve prolapse symptoms. Your doctor can refer you to a physiotherapist who specialises in women’s health. The treatment course usually lasts 3-6 months on average but you should continue regular pelvic floor exercises for life.
You can also do pelvic floor (sometimes called kegel) exercises at home from a young age which can reduce the likelihood of developing a prolapse later down the line.
Pelvic organ prolapse pessary
If your prolapse is more severe or causing symptoms, you might be offered a pessary. This is a device (either plastic or silicone) which is inserted into your vaginal canal to help support your pelvic organs. They come in different shapes and sizes.
Your healthcare professional will assess your prolapse and discuss which type and size of pessary is best for you. The first pessary you try might not always work for you straight away, but there are different options to try.
Once the right pessary is found for you, they can be changed and reinserted every 3-6 months, or you can learn to remove and reinsert the pessary yourself at home.
Pelvic organ prolapse surgery
Surgery is an option for prolapses that affect your quality of life and can’t be managed by a pessary or you do not want to use one. Like with any surgery, it comes with risks. If you have not completed your family, your doctor may advise you to delay your surgery as future pregnancies can increase your chances of a prolapse coming back. The surgery secures all the organs affected back into their right place. There is a 95% success rate with surgeries in reducing bulge-like symptoms(5).
Women may feel embarrassed to discuss pelvic organ prolapse, especially if it causes symptoms like leaking of urine. However, they are common and you are not alone. We’d encourage you to speak to your healthcare professional as treatment can be simple and make a big difference to your life.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.