I’m a women’s health GP with primary ovarian insufficiency
What's the lowdown?
Premature ovarian insufficiency (POI) is a condition that describes a woman who has reduced ovarian function far earlier than expected, aka you stop releasing eggs each month
1-3% of women before the age of 40 can have POI (2,6)
Symptoms are similar to menopause, but it isn’t the same as menopause
5-10% of those affected can still get pregnant (1,4)
It’s a huge diagnosis and can have a lasting impact on physical and mental health
Primary Ovarian Insufficiency and Me…
I’m Dr Nikki, a Lowdown doctor and GP specialising in women’s health. I also have premature ovarian insufficiency (POI).
I was diagnosed in early 2023 following a miscarriage the year before. To say it was the most devastating 2 years of my life is an understatement. I lost a whole part of who I thought I was and it took me a while to get to a new “normal” again.
Before my diagnosis I had NO idea what POI was. I have a background in gynaecology and obstetrics, yet POI had never been something I had knowledge of. Thankfully that has changed, and fast forward to 2024 and I am now an advocate for women experiencing this condition.
What is primary ovarian insufficiency?
Premature or Primary Ovarian Insufficiency is a term that describes an earlier than normal slow-down or lack of function in the ovaries that starts under the age of 40 years old. It can impact women as young as 13 if they don’t start having periods at all due to a genetic condition that affects their ovaries.
It can also be known as “early menopause”, “premature ovarian failure” or “premature ovarian aging” but these terms are no longer used because they don’t accurately or sensitively describe what is actually going on in a woman’s body.
What are common symptoms?
Period changes can be the first sign of a problem. After my miscarriage in 2022, my periods didn’t return to normal. They were prolonged and light. At one point I was bleeding for 3 weeks solidly. I felt like I was going crazy!
I also had perimenopausal symptoms, but I didn’t know it at the time. I was tearful, angry and grumpy – sometimes within the same day! I had to nap in the daytime, which isn’t usual for me, and I still felt tired when I woke up. I also had terrible brain fog and forgetfulness, and this still impacts me today even with HRT.
My sleep was bad too, I woke up multiple times in the night. I didn’t get night sweats, but I did have the odd hot flush in the day – they are not the same as normal sweating. I literally was dripping with sweat all of a sudden for no obvious reason.
Another sign was weight gain. I had changed nothing, but gained 10kg (about 1.5 stone). Looking back at my wedding pictures, it is obvious to me now that something was wrong.
Other symptoms people might experience include:
- Feelings of anxiety for no explicable reason
- Aches and pains in the joints
- Frequent urinary tract infections (UTIs)
- Loss of normal vaginal discharge
- Painful intercourse due to vaginal dryness
- Tinnitus
- Dizziness
- Palpitations
- Loss of interest/lack of motivation in everyday activities
How do you treat POI?
HRT – Hormone Replacement Therapy
The mainstay of treatment is HRT. Every woman diagnosed with premature ovarian insufficiency needs to be on HRT to protect her bones. I had a DEXA scan to check my bone health when I was diagnosed and discovered that I had osteopenia (bone thinning) in my spine. Without HRT, it is likely to progress to osteoporosis (more severe bone thinning), so I am super conscious of this and making a lot of effort to keep my bones strong through exercise as well.
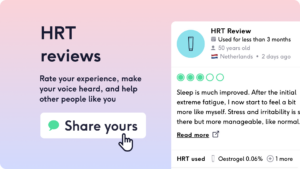
There are lots of ways HRT can be given, such as patches, gels, sprays or HRT pills and even the combined oral contraceptive pill can be used. Everyone is different, so it might take a few tries of different things before you know what is right for you. Using our HRT reviews can help you see what others have found useful, especially if you search for POI reviews.
Diet
While HRT is the main treatment, it can’t hurt to look at your diet. A healthy, balanced diet with everything in moderation is the best advice. Reducing alcohol intake can be helpful for reducing hot flushes. Reducing caffeine can also help with sleep and anxiety symptoms.
Lifestyle
The general advice is to stop smoking and ensure that you are exercising regularly. A suggested regime is 150 minutes of cardiovascular exercise per week and an additional 2x sessions of strength training to help your bones to stay strong. I attend yoga classes to help my mental health as well as my strength and flexibility.
Supplements
There is a lot you can do to help keep your body healthy overall with supplements. Taking Vitamin D supplements is an excellent way to keep your bones healthy. Aim for 400-800 international units of vitamin D per day. Some women also gain a lot from supplements like magnesium for sleep and muscle aches. Starflower oil can help with PMS-type symptoms.
How to manage your mental health with POI
My mental health took a massive hit when I received this diagnosis. I really struggled to see patients, especially those going through miscarriage or trying to conceive. I also had no motivation to do the things I normally enjoyed doing. It was like a piece of my brain had been removed and left a gaping hole that I’m steadily learning to refill.
You may feel like this too, so I urge you to get support. This can be through your GP and/or counseling. You’ll likely also have LOADS of questions, so a good resource to plug into is The Daisy Network. They have a supportive Facebook group and online group sessions to help answer your questions plus can offer you mental health support too.
When should you talk to your doctor?
If you are feeling symptoms of perimenopause or worsening PMS coupled with changes to your periods, or you’re struggling to get pregnant then the first place to go is your GP. At the very least ask for an FSH (follicular stimulating hormone) blood test to find out if your level is high. If the level is high (over 25), then you need another one 4 to 6 weeks later(2).
If it is abnormal, and you are under the age of 40, then this needs investigation and treatment. If your GP is not familiar, then point them in the direction of this guideline. If your GP can’t help, ask to be referred to a menopause specialist in your area or speak to Dr Nikki at The Lowdown.
You will need a bone scan and to start HRT which should be continued until at least the age of natural menopause (age 51). If you’re less than the age of 30, then I highly recommend you see a specialist for genetic screening as well to look for any underlying genetic cause of POI. This could be an endocrinologist or a gynaecologist, but should be a specialist who is experienced with POI.
Can I get pregnant with POI?
Studies have shown that around 5-10% of those with POI get pregnant, and we understand how emotive this is, especially if you’ve been diagnosed when young. There’s often pressure to do something about your fertility as soon as you’re diagnosed, but if you’re not in the right headspace for this, then there is no rush. Take time to process the diagnosis first and then explore fertility next. This diagnosis is not the end of your ability to have children. I am on an adoption journey with my husband at the moment! If this is not for you, there are other options like egg donation and IVF to explore.
Egg donation involves having IVF with someone else’s egg and your partner’s sperm. Many women worry that because the baby isn’t genetically “theirs” they won’t bond, but this is far from the truth. There is lots of research about how the environment of your womb actually changes how the genes of the baby are expressed (5), so they will be impacted by you and will be your child. The other added positive is that the success of this kind of IVF is based on the age and quality of the egg used, NOT on your age or your condition (5).
Before ruling out anything, speak to a fertility specialist to decide what your best course of action will be.
Where can I get help for POI?
Here are some resources I recommend to learn more about POI and get support:
If you’re into reading, try My Life on Pause by Dr Siobhan O’Sullivan.
If you prefer to listen to discussions from women going through similar, try the new podcast “The Premature Menocast” featuring me, Dr Nikki, on Spotify.
And finally, there is a great support group called The Daisy Network.
I also recommend that you get stuck into The Lowdown’s Perimenopause Review Platform and read about other women’s experiences, and leave your own to help others when you feel ready to.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.

