
Do I need to give my body a break from contraception?
In this article
What's the lowdown?
Combined hormonal contraception methods (the combined pill, patch and vaginal ring) may include a four to seven day break, but some users wonder whether they should give their body a longer break from hormonal contraception.
There is no medical reason for most of us to have a long-term break from our birth control.
Some individual circumstances, like age, family history and future plans, might mean that a break, switching or stopping hormonal contraception altogether is a good idea.
Long-term use of hormonal birth control does not affect your fertility.
Your risk of blood clots could increase if you stop taking combined hormonal contraception and then restart it again after more than four weeks.
Combined hormonal contraception can increase your risk of breast and cervical cancer, but can decrease your risk of endometrial, colorectal and ovarian cancer.
If your medical circumstances change, you might be advised to stop, switch or have a break from your hormonal contraception.
If you’ve been on hormonal contraception for a while, you might be wondering whether it’s time to take a break. This is a common concern that many people have, possibly because they’re noticing side effects, are thinking of trying for a baby or just want to try a different method. There are loads of reasons you might want to take a breather from your contraception. But the question is: do you need to?
First of all, let’s set out exactly what we mean when we talk about taking a break from contraception. Combined hormonal contraception users of the pill, patch and vaginal ring may have a four to seven day break from their chosen method every month, but evidence shows that this is not necessary.
We’ve created a full breakdown on back-to-back pill-taking, however in this article, we’re going to talk about what the science says about longer pauses: stopping off your hormonal contraception for more than a week or two.
What happens when you take the pill for a long time?
Some people worry that taking their hormonal contraception continuously for a long period of time – several years – will cause a build-up of hormones in their body, and that a break will help to ‘reset’ things.
Others worry that their body is working harder on the pill, or is being put under stress from the hormones some contraceptives contain. These are logical doubts and it’s great to think about the way our contraception is affecting us. However, once we understand how the pill works, it’s reassuring.
Most methods of hormonal birth control work to stop ovulation, preventing fertilisation of an egg and as a result, pregnancy. The hormones in birth control that make this happen pause the menstrual cycle. A daily dose of the pill is required to achieve this so there’s no build-up of hormones, and our body is actually having a break from ovulation when we’re on hormonal birth control.
There’s one particular rumour (aka myth), and it’s a question we get asked a lot here at The Lowdown. Should you have a break from the pill after 10 years? There’s actually no evidence to show that this is beneficial at all, and your doctor will usually tell you that you can keep taking the pill for as long as you want to and it is safe for you to do so. There may actually be some risks associated with stopping and restarting the pill, which we’ll dive into now.
Going back to the pill after a break
There are many reasons you might want to take a break from the pill, and we’ll look more into those in a moment. But if you’re here simply because you’re wondering whether a break would be good for you, and you don’t have any other reasons for stopping (like side effects or trying for a pregnancy) research tells us the answer is no.
Fertility
As birth control’s main goal is to stop you from getting pregnant, it makes sense to wonder whether taking it for a long time will impact your fertility. In reality, though, research has shown that those who have stopped taking hormonal contraception have very similar levels of fertility to those stopping other forms of contraception, like condoms.
In fact, several studies have found that fertility is not affected by the type of contraception you were taking before you stopped.
Risk of Blood Clots
There is an association between oral contraception and blood clots. Understandably, many of us are concerned about these risks. Before you start oral contraception, you should speak to a doctor (we’ve got some lovely ones who can talk things through with you) about your personal risk factors for blood clots, such as smoking, family history and BMI.
If you take a combined oral contraceptive pill, like Yasmin or Millinette, your risk of blood clots is highest when you are just starting your contraception. In these cases this may be because taking a combined hormonal contraceptive can uncover any clotting issues you might naturally have.
Research has shown, however, that your risk of blood clots is increased again if you stop taking combined hormonal contraception for four weeks or more and then restart it again.
Cancer
There is evidence to show that the use of combined hormonal contraception could increase your risk of cervical and breast cancer, but this increased risk is small and reduces with time after stopping. One study showed that any increased risk of cervical cancer declines once combined hormonal contraception is stopped, but could take longer to reduce in long-term users.
This might sound scary, but other research shows that those who take oral hormonal contraception, or have taken it in the past, have a reduced chance of developing cancers such as womb (endometrial) cancer, ovarian cancer and colorectal cancer. The risk of developing both endometrial and ovarian cancer reduces the longer you take hormonal contraception.
It is a good idea to look at your family history to see whether you are likely to have a naturally higher risk of developing a certain type of cancer. Your doctor will be able to talk this through with you in more detail.
When should I have a break from my contraception?
There are some scenarios which might mean that a break from your contraception – or stopping it altogether – is the right choice for you.
Age
The risks we mentioned above are minimal for most contraception users, and the benefits of hormonal contraception use are often greater than the risks. That being said, there are some situations in which the risks associated with hormonal contraception could actually outweigh the benefits. Generally those over the age of 50 are advised not to use combined hormonal contraception for this reason.
With age, women tend to be at increased risk of osteoporosis, a medical condition where the bones become brittle and fragile. The injection is linked with a small drop in your bone mineral density which recovers when you stop using it, but for some this may mean the contraceptive injection, such as Sayana Press is a less suitable choice as they get older.
Planning a family
If you are thinking of starting a family, you’ll want to stop taking your contraception altogether. If you take hormonal contraception for reasons other than pregnancy prevention, or have had a baby already and are looking at restarting your contraception, we’ve got a great article that covers everything you need to know.
Side effects
Usually, any negative side effects you experience from hormonal contraception will lessen the longer you stick with it. It’s unlikely that you will develop new side effects after taking a particular birth control for a period of longer than a few months, but if you think this is the case for you it might be worth having a chat with your healthcare professional.
If you are trying a new hormonal contraception, though, or have tried several and are experiencing unwanted side effects, you may want to consider switching to a different method.
Switching contraceptives
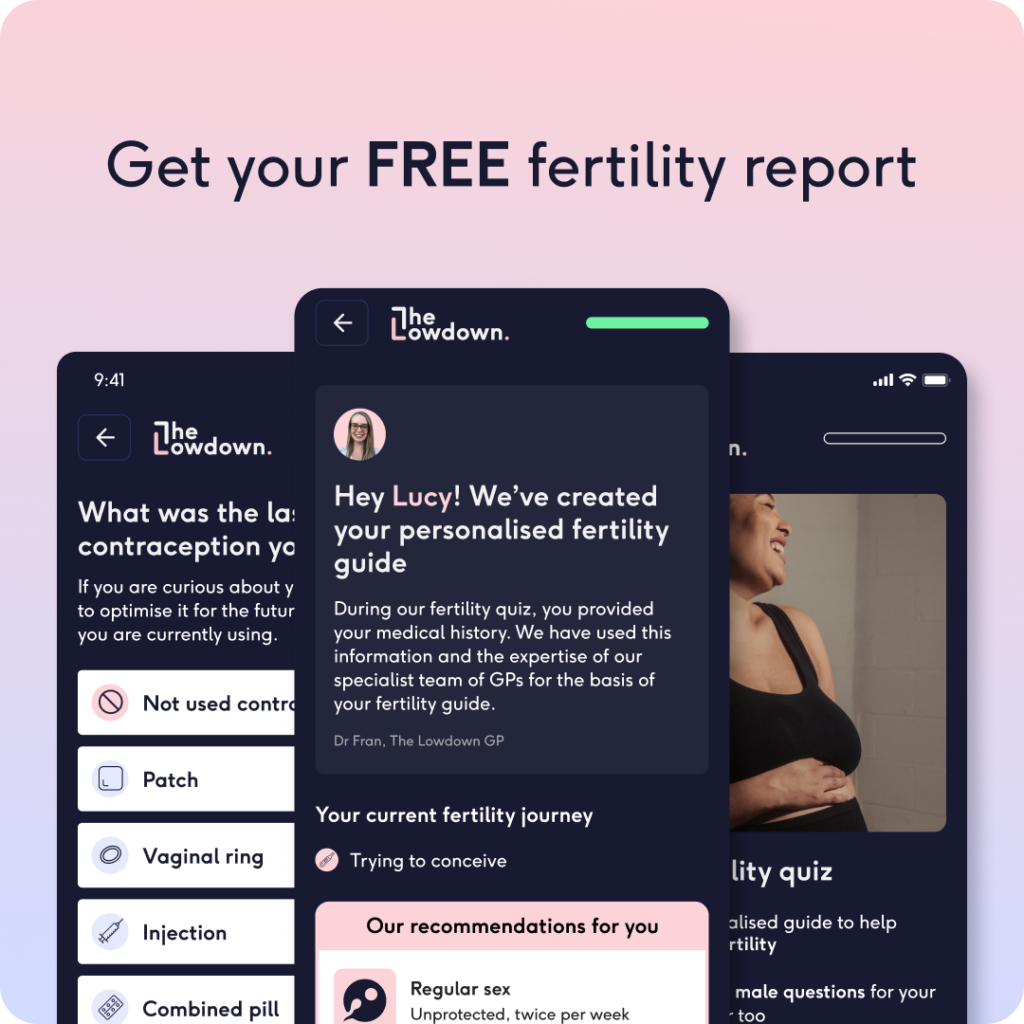
If you do decide to switch your contraceptive method, there are lots of options for you to choose from. You don’t need to have a break between hormonal contraception methods, and can move straight onto non-hormonal alternatives if you find that hormonal contraception isn’t working for you. Use our contraception comparison tool to directly compare two methods, or take our contraception recommender quiz to find a method that could work best for you.
Following your doctor’s advice
In some cases, your doctor may advise you to stop taking hormonal contraception. This could be due to a number of factors, such as your weight, smoking status or family history of cancer or blood clots. These cases are highly individualised, and the best alternatives will vary from person to person.
So should you take a break from the pill?
In short, unless your individual circumstances suggest that you should, you do not medically need to give your body a break from hormonal contraception. This applies to all hormonal contraception, be it combined hormonal contraception methods like the pill, patch, or vaginal ring, or progestogen-only methods like the mini pill, implant, injection or hormonal coil. As long as you’re feeling well, and your method is considered safe and working for you, you can use it for as long as you want!
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.






