
What can you do to stop heavy periods?
Disclaimer: This article is sponsored by Evana, but just like all of our other content, this is a completely honest breakdown. See our Content Policy for more details.
Heavy periods are a nuisance. For many reasons – not only the constant self checking for fear of leakage, bloodstains and embarrassment, but also the extra added cost of period products and even the risk of anaemia. FYI – anaemia is a medical condition where your body doesn’t have enough healthy red blood cells to carry oxygen around the body.
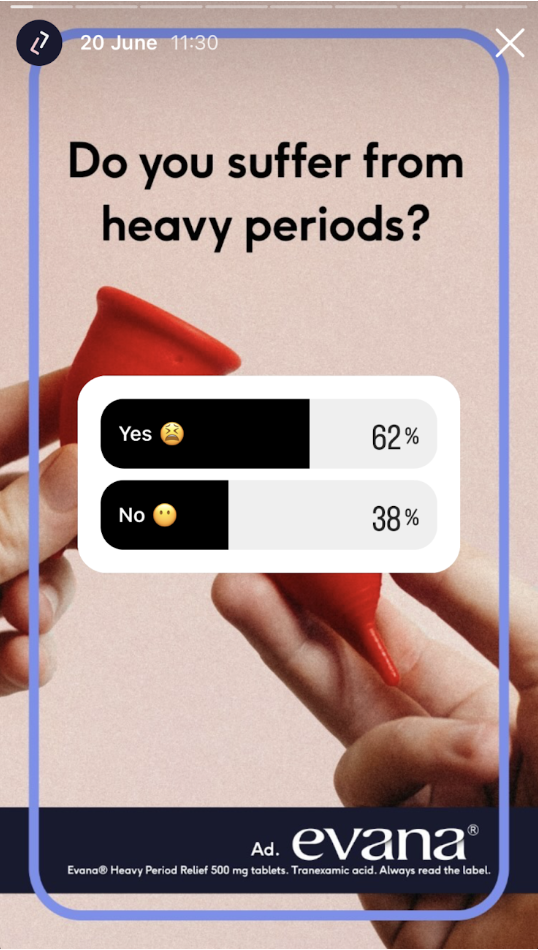
Heavy periods are common, affecting around 10% of us1, and even up to 37% of adolescents2. But amongst our Lowdown Instagram community – it’s a whopping 62%!7 So we thought you should have a handy guide covering the what, why and how of managing troublesome bleeds.
What is a heavy period?
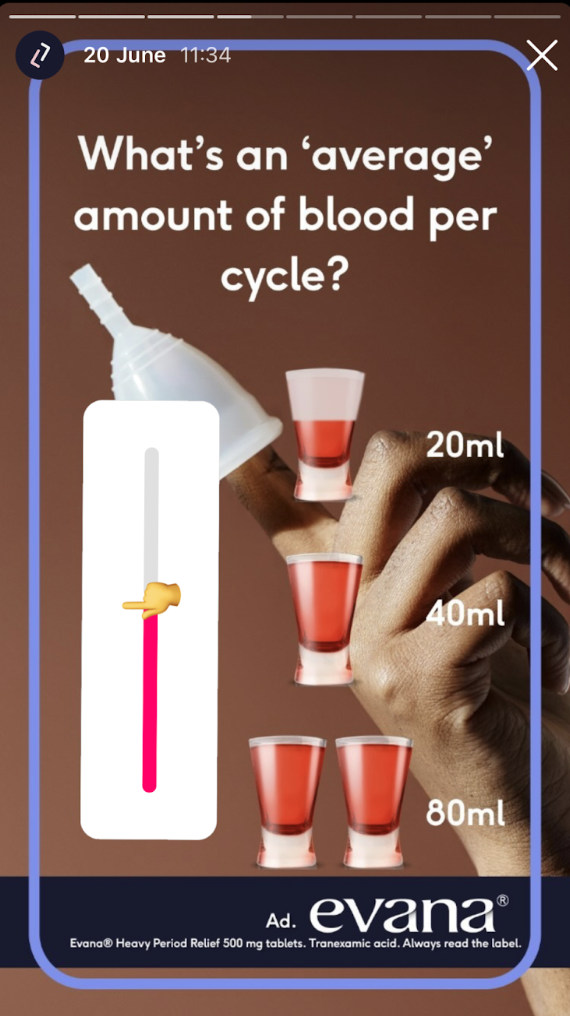
The technical medical term for heavy periods is “menorrhagia”. Heavy periods are defined as blood loss of 80 ml or more over a cycle, which is quite hard to quantify if you ask me, so here is a list of signs and symptoms which identifies heavy periods without having to wring out your period pants.
- Changing your period product more often than you should – aka every one to two hours for a pad or tampon or more often than the recommended length for products like a menstrual cup or period pants
- Needing to double up on period products, for example, using a tampon and pads or period pants at the same time
- Periods that last for more than seven days
- Passing blood clots that are bigger than a 10p coin (which is 2.5cm as we’re increasingly a cashless society!)
- Bleeding through your clothes or bedding
- Feeling tired or out of breath which can indicate that you have anaemia due to your heavy periods
- Avoiding your everyday activities, like exercise or work
One in 20 women between the ages of 30 and 49 see their GP each year due to heavy bleeding and period problems2. And studies have shown that many women who see their GP don’t meet the criteria for heavy periods of 80 ml blood loss per cycle. This is why the definition used by doctors now takes into consideration the impact of bleeding on your life to ensure that people whose periods are affecting their quality of life are included in treatment guidelines.
What causes heavy periods?
Half of all people with heavy periods will never have a cause found – frustrating, but it’s women’s health so we’re used to it! For the remaining half who have an underlying cause for their bleeds, they are usually due to one or more of the following:
- Fibroids
- These are benign (non-cancerous) growths found within the layers of the womb. Fibroids are made of fibrous tissue which is made from the cells usually found in muscles, tendons or ligaments.
- Endometrial polyps
- These are benign growths on the inside of the womb made from cells that are the same as the womb lining.
- This is where tissue similar to the lining inside the womb, known as the endometrium, starts to grow outside the womb. Read more about endometriosis.
- Adenomyosis
- This is where the tissue that lines the inside of the womb can be found deep in the muscle of the womb.
- This is a condition affecting your hormones and how your ovaries work. Read more about PCOS.
- Perimenopause describes the time during your life before menopause, when your periods eventually stop. Read more about perimenopause
- Pelvic inflammatory disease (PID)
- This is an infection of the female reproductive system including the womb, fallopian tubes and ovaries.
- Medications
- These include SSRIs (selective serotonin reuptake inhibitors, a type of antidepressant), anti-coagulants (blood thinning medication) and the copper coil (IUD).
- Other conditions including clotting disorders, hypothyroidism or diabete
- Rarely, cancer of the womb, ovary or cervix
What are the risks of heavy periods?
Physically, heavy periods mean you lose more blood. And if you can’t replace that blood quickly enough before your next cycle, you’re at risk of iron deficiency anaemia, where your body lacks iron to produce enough healthy red blood cells to carry oxygen around your body. This can make you feel, frankly, rubbish. Anaemia can cause fatigue, shortness of breath, headaches, palpitations, and hair loss, but if it’s severe, you’re even at risk of chest pain and collapse – so catch it early, as iron is easy to replace and you’ll feel tons better for it. Heavy periods can also have a huge effect on your social life, career and confidence if you’re regularly flooding through clothes or worrying about when to next change your products.
How can I treat heavy periods myself?
The NHS and healthcare services are stretched, we know. But there are steps you can take while you’re waiting for your first GP appointment, or while you are on a waiting list to see a gynaecologist, which don’t require a doctor’s input.
Firstly, you can try medications that don’t need a prescription and you can buy from a pharmacy. Anti-inflammatory medications like ibuprofen and naproxen can help reduce blood loss. Naproxen can be bought from the pharmacy under the brand name Ultravana.
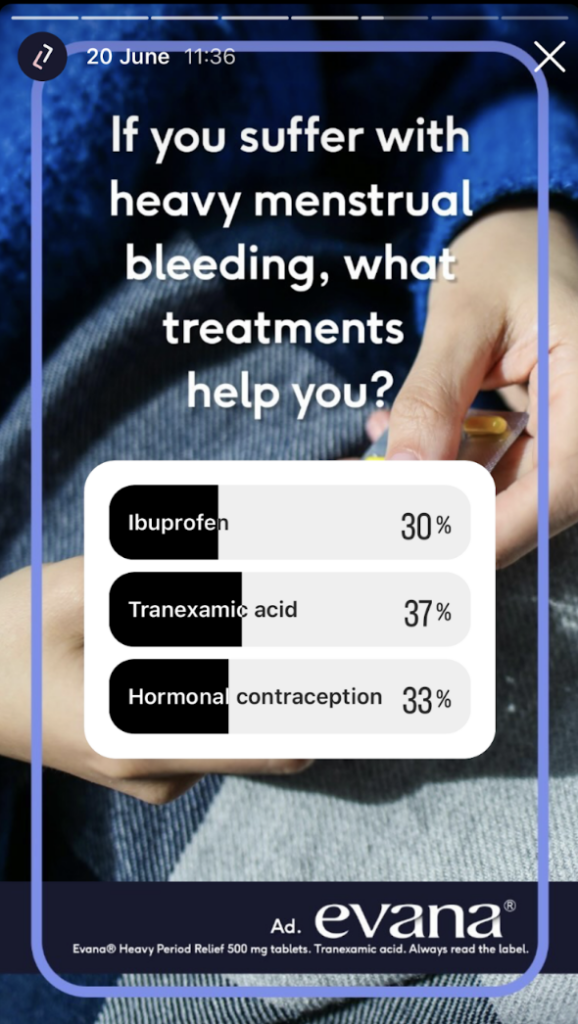
Tranexamic acid is a medication which helps your blood form clots, so reduces blood loss. Evana is the only brand of tranexamic acid which is available from a pharmacy. You can buy it without a prescription if you are aged between 18 to 45 and have a regular cycle. It can be taken for up to four days from the first day of your period and is the number one non-hormonal treatment recommended in guidelines. And guess what – in our Instagram poll, 37% of our users said tranexamic acid helped with their heavy periods compared to 30% who found ibuprofen useful and 33% who used hormonal contraception to help.7
Secondly, don’t wait for anaemia to take hold, start upping your iron yourself. In fact, people aged 19 to 49 who are having periods are advised to have almost double the amount of daily iron compared to those who don’t bleed5. Iron rich foods include red meat, beans and nuts, but you can also buy supplements from many supermarkets and pharmacies. Be warned though, that iron supplements can cause some really interesting side effects – either constipation or diarrhoea and often black poo! Iron is absorbed much better in your gut if you take it with vitamin C (found in citrus fruits and even broccoli) and isn’t absorbed well if you wash it down with a cup of tea!6
How should I talk to my doctor about heavy periods?
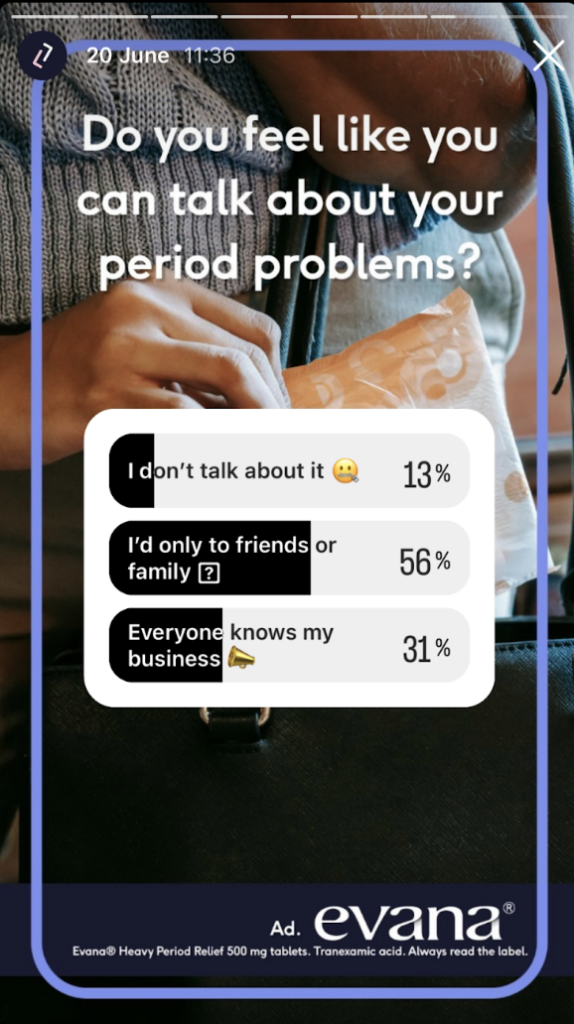
56% of our users speak to friends and family about their heavy periods….but please, speak to your doctor too. Doctors love it when you are straight with them. So start the appointment by explaining that you have heavy periods and how they are affecting you. It’s really useful to write down your average cycle length and how many days you bleed for. And if your cycles are irregular, tell them that too!
Your doctor will probably want to examine you and arrange some blood tests to look for a cause of heavy periods and to check for anaemia. Some people may be referred for a scan of the womb .
After a cause has (or often hasn’t) been found, you and your doctor will be able to have a better idea of which treatment option may be best for you.
What are the treatments for heavy periods?
Treatments broadly fall into three categories:
- Non hormonal treatments
- These are anti-inflammatory medications like ibuprofen or Ultravana, or tranexamic acid, such as Evana.
- Hormonal treatments
- You’ll usually be offered the hormonal coil first, and one that contains 52mg of levonorgestrel as this has the best evidence for reducing blood loss from heavy periods.
- If this isn’t suitable then other hormonal options are the combined pill which you can also take continuously without a break to avoid withdrawal bleeds, or synthetic progesterones that are taken every cycle.
- You could also consider the progestogen only pill, injection or implant as these do stop periods or make periods lighter for some. However, bleeding patterns on these methods are unpredictable and there is the chance that you can bleed more regularly or even more heavily on these options.
- Surgical treatments
- These include surgical procedures such as uterine artery embolisation, myomectomy, endometrial ablation or even hysterectomy (removal of the womb) depending on the cause of the heavy bleeding.
Hopefully this short guide has helped give some pointers on how to manage your bleeds. And please don’t let them stay heavy on your mind – start managing them yourself today and book a GP appointment for more support.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.






