The stages of labour and birth
In this article
What's the lowdown?
There are 3 stages of labour
The first stage refers to when your cervix is slowly ripening and opening
The second stage is the birth of your baby
The third stage is the delivery of the placenta
Baby, it’s time to meet your little one! It’s been 9 months of growing and nurturing, you can’t wait to meet your new addition to the family.
Labour isn’t as straightforward as pushing the baby. There are actually different stages of labour, all equally important in helping guide the baby out of the womb (uterus) into the real world.
Latent stage of labour
When your cervix (the neck of the womb) starts to soften and slowly open, this is referred to as the latent stage of labour. It is when the cervix is between 1cm to 4cm dilated (opened).
You might not necessarily feel contractions but they might come on and off, without a regular pattern. This is not quite the start of labour and it might take hours or even days before you are in established labour (more on this below)1.
Try and stay lightly active as it can help the baby move down the pelvis, slowly putting pressure on the cervix, and helping it dilate. Ensure you are eating and drinking, gathering as much energy as you can before you enter the established labour stage1.
First stage of labour
You might hear this being referred to as established labour. They are the same.
Once your cervix has reached 4cm in dilation and you’re feeling regular strong contractions, congratulations you have made it to the first stage of labour1.
Hold off rocking up to the hospital or calling your midwife just yet. Wait until you1,2:
- Feel regular contractions at least every 5 minutes
- Felt your waters breaking
- Experiencing painful contractions that are becoming unmanageable without pain relief
- Feel like something is wrong
Once you are admitted to hospital, your doctor or midwife will offer regular vaginal exams, typically every 4 hours, to track how quickly your cervix is dilating. This is a good indicator of how your labour is progressing1.
Your cervix needs to dilate fully to 10cm before you can start pushing. You might feel the urge to push but do not do so before your healthcare professional gives you the green light.
If this is your first baby, you can be in established labour for 8 to 18 hours. Subsequent deliveries can be faster, around 5 to 12 hours on average1.
Sometimes things can take a little longer than anticipated so you might need a helping hand. You could either be offered for your waters to be broken artificially or a hormone (oxytocin) drip1.
Breaking of waters
If your water (membrane holding the amniotic fluid around your baby) is still intact, you could be offered an artificial rupture of membranes (ARM). It is thought that without the waters, the contractions might become stronger or more regular. Your doctor or midwife may suggest some stronger painkillers to combat the pain1.
Hormone (oxytocin) drip
An ARM might not work so the alternative is using a synthetic version of the oxytocin hormone. This is the hormone that makes your uterus (womb) contract and the drip should make the contractions stronger. You will be given this through an intravenous injection via the vein in your arm1.
Again, as your contractions tend to get stronger and more regular with the drip, your doctor or midwife will discuss strong pain management options with you. As this is quite a strong medication, you will need regular monitoring of the baby’s heartbeat and vaginal exams1.
Second stage of labour
This is when your cervix is fully dilated to 10cm and your body is ready for pushing. Your midwife or doctor will help you find a comfortable position to give birth and can offer some suggestions like positioning your legs to make it easier for you. Many baby mamas choose to lie on their back but you can also lie on your side, stand, kneel or squat1.
With each contraction, your baby is slowly moving down the vaginal canal. You should push every contraction but it is also important to push correctly. You might hear your team say “push as if you are doing a poo”. If you have an epidural (a form of painkiller), you might not feel an urge to push so your healthcare professional will monitor your contractions and guide you when it is the right time to push1.
Your birth partner can stay right next to you to offer moral support in this miraculous journey.
The second stage of labour is not instantaneous and can sometimes last hours. First pregnancies are allowed 3 hours to push but it is 2 hours for those who have had children before. If you exceed this time limit, your team might need to reassess the situation and help the baby out either with a forceps or suction cup1.
Episiotomy
If your baby is struggling to leave the vaginal canal, your doctor or midwife might suggest an episiotomy. This is a small cut of the skin between the vagina and anus which allows more room and reduces the chances of tearing around the perineum (area between the vagina and anus)1.
Don’t worry, you will be given some numbing medication (local anaesthetic) so you cannot feel the cut. Afterwards, it will be stitched up by a professional and the healing can be checked by your midwife and at your GP postnatal check after birth.
Third stage of labour
Baby is here, time to celebrate! Well yes, but we still have one thing left to do, deliver the placenta. This can be done either with treatment (active management) or naturally (physiological management). In some cases, either method does not work and the placental needs to be manually removed by a healthcare professional.
Treatment (active management)
Oxytocin, a naturally produced hormone in the body, makes your womb contract more. So this hormone is injected into a muscle (similar to a flu jab) to encourage your womb to contract and detach from the uterus wall1.
The umbilical cord is not cut straight away, usually, we let 1 minute or more pass before snipping away as it is shown to have benefits for the baby (increasing iron levels). Once the placenta has come away from the uterine wall, your midwife will slowly guide the placenta out of the body through the vagina by tugging at the umbilical cord. Ideally, this should be completed within 30 minutes of the little one being born1.
Active management of the third stage of labour does reduce the risk of post-delivery bleeding (postpartum haemorrhage). But this might make the contractions worse1.
Natural (physiological management)
Unlike active management, no medications are given. The cord is not cut until it stops pulsating, allowing blood to flow from the placenta into the baby. The placenta will naturally come away from the womb lining, indicated by a small gush of blood. You will then have to push, kind of like pushing a baby out. The pushing will only last several minutes but it can take up to an hour for the placenta to separate from the wall3.
If things aren’t happening naturally, you might be advised to try some oxytocin.
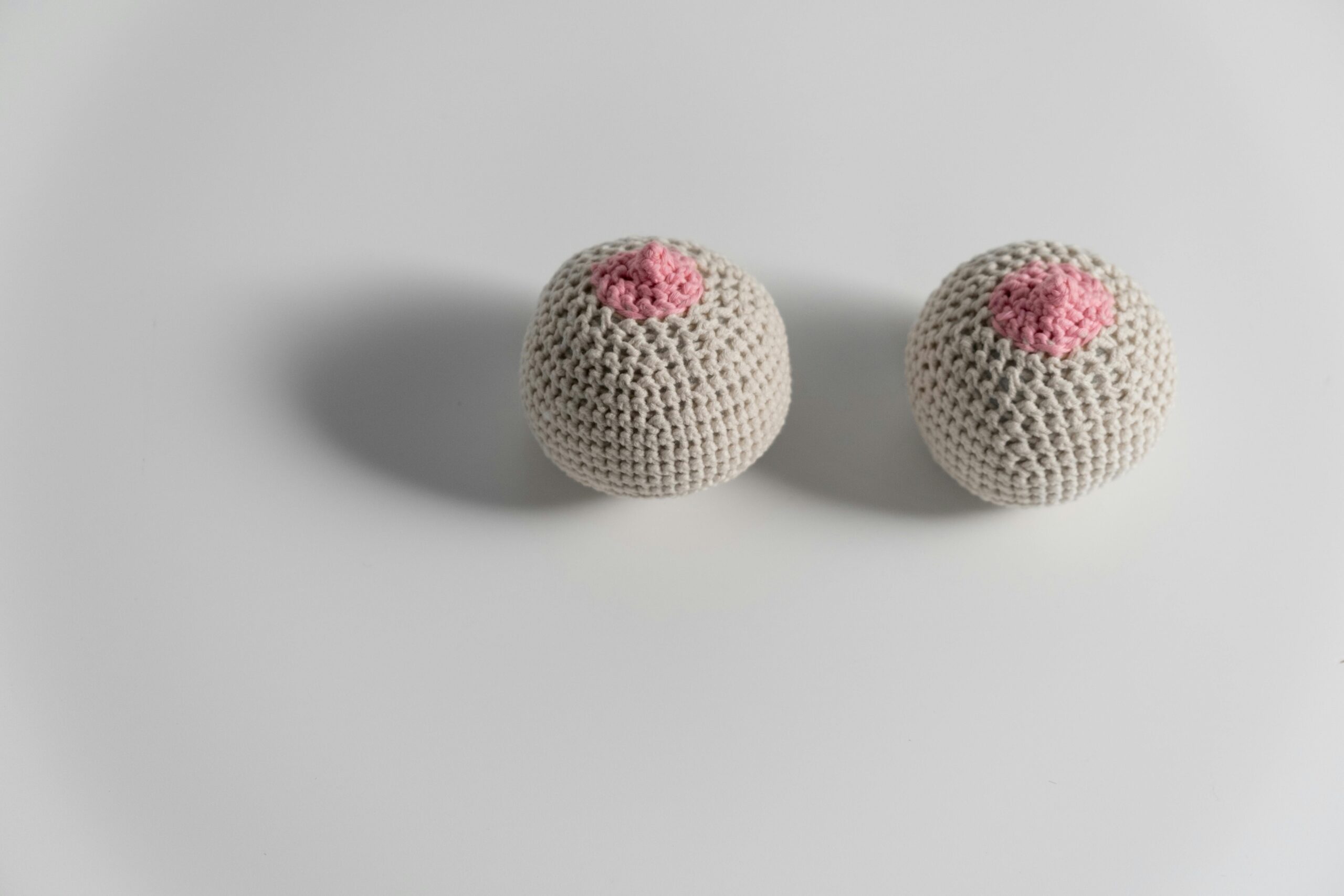
Baby is born
Once your baby is here, you should be able to hold onto your little one straight away and enjoy some quality skin-to-skin contact. Whenever you are ready, you can start breastfeeding but ideally, this should be done within 1 hour of birth.
Sometimes, your baby may need some help with breathing after they are born and will be assessed by a neonatologist (specialist in newborns) who will decide what follow-up care they will need.
Fourth stage of labour
This refers to your recovery after delivery. You may need to have some monitoring, stitches around your perineum or treatment for heavy bleeding. During this time, it’s important to rest and enjoy the greatest cup of tea and slice of toast you will have ever had.
And finally, congratulations!
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.