Progestogen-only contraception and breast cancer – what’s the risk?

This guide has been peer reviewed by the medical team at The Lowdown and the FSRH and is regularly reviewed as per both clinical content policies
In this article
You may have seen the article published on BBC news ⁽¹⁾ about the new study ⁽²⁾that links the progestogen-only contraceptive methods to an increased risk of breast cancer. Let’s unpack the study and what this means for you if you’re taking the mini pill, injection, implant or hormonal coil (IUS) .
What we knew about hormonal contraception and cancer
We already know that there is a small increased risk of breast cancer if you’re taking the combined pill – for example, Microgynon, Yasmin and Lucette, which contain oestrogen and progestogen.
However, most of the research so far looking at progestogen-only contraception and breast cancer risk has been inconsistent or looked at all hormonal methods, grouping progestogen-only and combined contraception together which made it really tricky to definitively say whether or not progestogen-only methods affect breast cancer risk.
Now finally, someone has researched progestogen-only methods! This is great news, and the results aren’t too alarming.
What is the study and is it legit?
The study was published in the PLoS Medicine journal on the 21st of March and looked at nearly 30,000 patient records held by GPs in the UK, including almost 10,000 women under 50 years old who had breast cancer diagnosed between 1996 to 2017, and a control group….so it’s pretty legit.
What does the study tell us?
The study revealed that similarly to the combined pill, current or recent users of the progestogen-only / mini pill, injection or hormonal coil (IUS) were found to be at slightly increased risk of breast cancer. When this data was combined with earlier published studies, the authors found a similarly elevated risk associated with the progestogen implant. There was no significant difference between the types of progestogen-only methods and their effects on breast cancer.
The results of the study showed that women who used any method of hormonal contraception had a 20-30% higher likelihood of developing breast cancer compared to those who did not use hormonal contraception.
That sounds concerning, however it’s really important to stress that the risk of breast cancer in women of reproductive age (i.e. users of contraception) is small and breast cancer is rare in younger women under 30⁽³⁾. So a 20 to 30% increased risk in this age group means a small number of extra cases of breast cancer.
Let’s break it down: for every 100,000 women who are aged 35-39, which is the size of the population of Worcester, 265 more women who have been using oral contraceptives, so combined or progestogen-only pills, for 5 years could develop breast cancer in the next 10 to 15 years. The risk is smaller in younger women suggesting an extra 61 women per 100 000 aged 25 to 29 years old and an extra 8 women per 100,000 aged 16 to 25 years old will develop breast cancer.
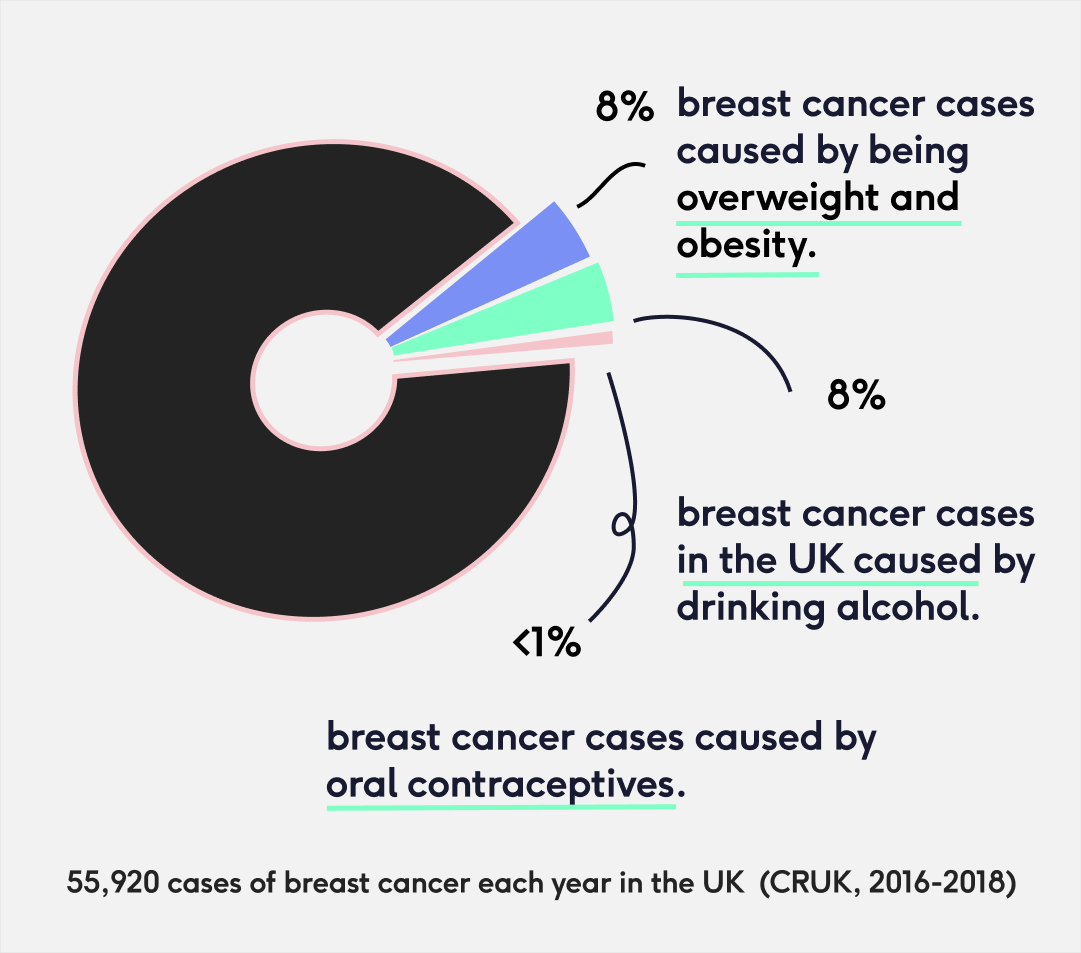
Let’s put this into perspective: there are almost 56,000 cases of breast cancer each year in the UK of which 8% are caused by obesity and being overweight and another 8% are caused by drinking alcohol. Less than 1% are caused by oral contraceptives ⁽³⁾.
We also have to balance this against the well-known benefits of hormonal contraception, which prevent unplanned pregnancy and help manage often debilitating conditions such as heavy or painful periods, endometriosis, PMS, PCOS and acne, and which have a protective effect against womb and bowel cancer.
Am I still at risk if I’ve stopped taking these methods?
The risk is likely to decline after you’ve stopped using the injection, implant or hormonal coil (IUS) and the study found that 10 years after stopping oral contraception, your risk will go back to normal.
Hopefully, this blog has explained the study further, but if you have any other questions or concerns, don’t hesitate to reach out to us or speak to a doctor.
What does the study not tell us?
They recorded prescriptions during a defined period only meaning that they don’t have information on progestogen contraceptive use prior to the start of the observation period, making it difficult to assess the long-term impacts of contraceptive use or the total duration of contraceptive use on breast cancer risk.
Does the breast cancer risk change anything for you if you’re taking progestogen-only contraception?
Previously, there was a gap in the knowledge on the effects of progestogen-only contraception on breast cancer. However, our assumption that if there was a slight risk, it would be small, seems to be supported by the study.
Therefore, we don’t think there’s any cause for immediate concern and it’s unlikely the findings from this study will change who can and can’t use progestogen-only contraceptive methods. For most people the benefits of hormonal contraception will far outweigh the risks.
However, individuals who have current breast cancer should not use any form of hormonal contraception and those with a past history of breast cancer would usually only do so in consultation with their oncologist and cancer team.
Am I more at risk of breast cancer on progestogen-only contraceptives, if I have a family history of breast cancer?
Everyone has BRCA genes, which protect us against breast and ovarian cancers. Some people have a faulty BRCA1 or BRCA2 gene, meaning this protective effect doesn’t work as it should. If you know that you have a faulty BRCA gene, combined contraception is not generally advised as you are already at a higher risk of developing breast cancer. Guidance in the UK advises that progestogen only methods are generally considered safe for people with a BRCA gene mutation to use ⁽⁴⁾. This new study hasn’t changed any current guidance for women who carry the BRCA gene, but at The Lowdown, we’re going to keep an eye out and let you know if any changes to guidance are made in the future. In the meantime, if you’re worried, you can speak to a doctor for advice.
Having a family member with breast cancer does not necessarily increase your risk. 1 in 7 women ⁽³⁾ in the UK will be diagnosed with breast cancer so it is not uncommon to have someone with breast cancer in your family. However, if you have a significant family history of breast cancer or other cancers, or family members who have been diagnosed at a young age, speak to your doctor who will be able to advise you about the need for genetic testing ⁽⁶⁾.
Why does the mini pill increase the risk of breast cancer?
We’re still unsure about why hormonal contraceptives increase the risk of breast cancer. However, we do know that the hormones oestrogen and progestogen can cause some breast cancers to grow. We know breast cancer risk is influenced by your lifetime exposure to reproductive hormones. In fact, factors like starting your periods at a younger age and going through the menopause at an older age can increase your risk of breast cancer. Having children and having them at a younger age can decrease the risk ⁽³⁾.
This blog can help you learn more about various contraception options, but it does not give medical advice. You should always speak to a nurse or doctor when making choices about contraception and before starting a new method.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.