by Dr Melanie Davis-Hall · Jan 26, 2022

For those of you who don’t know I’m a GP by background and alongside the lovely Dr Fran I am one of the Lowdown’s Medical Directors. It was lovely to see all your faces at our WCD event, especially after remote consulting for 18 months, and getting the chance to meet some of you who’ve had appointments with us, worked on our content, or helped to build our amazing community. By the time you read this we’ve probably learnt even more about these topics so be sure to check out our blogs and event pages for more insights!

The Lowdown on medical research and contraception
We’ve all realised how traditional research has its limitations – you have to have large studies that are rigorously designed to be valid and its slow. Research on contraception and women’s health can be difficult. Hormones and hormonal contraception are complex areas of science with contradictory effects on the body which are also ethically tricky to study. It also takes time for new research and emerging evidence to filter through to the medical community and to become accepted practice.
This doesn’t quite fit our fast paced tech age and there’s a tension there. If there’s new advances in medical knowledge, clued up contraception users want to know about them, maybe even before this filters through to medical practice. But the medical community tends to be more cautious and it takes time to change the status quo.
We as health professionals and users of contraception have to recognise this tension exists and work with it. This is where The Lowdown excels. Rather than turning to Mumsnet forums, contraception users can research the evidence and discuss their experiences all in one place. We as doctors have to learn to interpret evidence alongside our patients and share the limitations of research honestly – which is what we’ve been trying to do with contraception at The Lowdown.
Through this we’ve learnt and are still learning what’s important to women and users of contraception, where the status quo does not address this and what’s important we focus on for the future. I’m going to talk about how The Lowdown has grown to embody and fight for this and share with you some examples of how our community has educated us in all things women’s health!
D-Mannose and UTIs
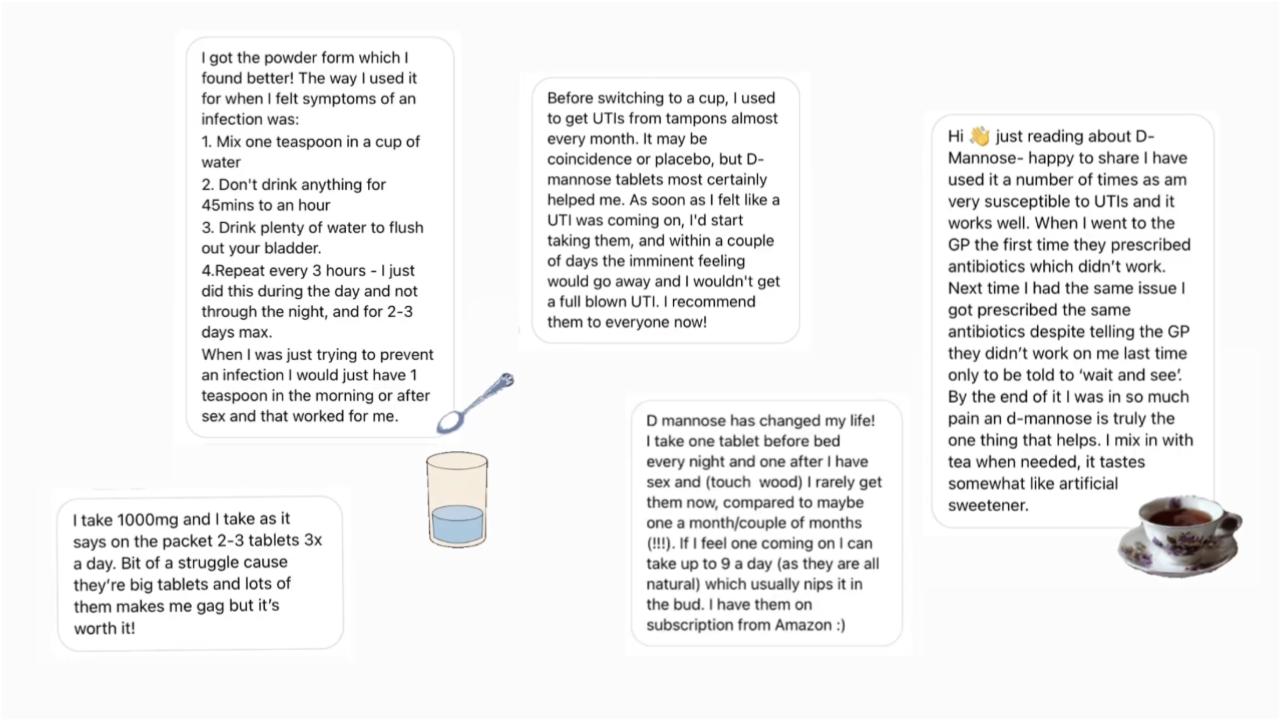
We did a Sunday surgery with the wonderful @selfcaredoctor Dr Masarat about urine infections, aka UTIs, and we were inundated by lots of you telling us all about D-mannose, a sugar that is available to buy as powder or tablets; and is not a medicine, but which many of you had found helped with keeping recurrent UTIs at bay.
There are a small number of studies on a small number of people showing promising results for D-mannose in UTI prevention. With results better than placebo and likely equal to antibiotics, and few side effects, it is now recommended by bodies such as the National Institute for Health and Care Excellence and Public Health England as a self care option non pregnant women may wish to try.
We’re awaiting the results of an Oxford university Randomised Controlled Trial (gold standard study) to evaluate whether D-mannose helps women suffering with recurrent UTI presenting to their GP and its cost effectiveness.
Paused egg syndrome
We ran an online event on Polycystic Ovary Syndrome (PCOS) with world-leading reproductive health expert, Professor Colin Duncan, a few months ago. The event was fascinating and we learned that PCOS doesn’t cause cysts, but actually hormonal imbalances cause eggs to pause in their development and these look like cysts on an ultrasound scan. For the most common reproductive disorder in the world, it’s really an overlooked fact!
It was also interesting to hear about his tests on sheep which are showing that the condition may be caused by exposure to excess testosterone before we are born. And whilst we have been lacking evidence that PCOS by itself can cause weight gain, or that having PCOS makes weight loss difficult or impossible, Prof Duncan’s research on sheep shows that PCOS may affect insulin signalling in such a way that burning of calories is more difficult. Something which resonated with many of you and really makes us think about how little we know about hormones and metabolism!
All of our webinars are recorded, so you can watch it back at any time.
Coils and pain on fitting
In the wake of Naga Munchetty and Caitlin Moran sharing their experiences of pain during coil fittings, you took to social media to tell us about your experiences. For most women the experience of having a coil fitted may be unpleasant and crampy but tolerable. For some women, however, the procedure can be excruciatingly painful and sadly lots of you reported undergoing painful coil fittings and some without pain relief.
The reasons for the variation in experience of pain are many but are usually fairly unpredictable. There is however strong evidence behind the value in offering pain relief. We looked at the research and found that only 25% of clinicians routinely use local anaesthetic when fitting coils, and 25% never use it. Lidocaine sprays and numbing creams have been proven to reduce pain significantly and in our opinion pain relief should be routinely offered to everyone being fitted with a coil. Guidance for healthcare professionals has since been updated, but as we know changes take time to filter into practice so we have developed a guide for you!
Importantly, greater anxiety, greater anticipated pain and negative perceptions of coils and coil fittings prior to the procedure appear to correlate with higher experienced pain scores in the research. We certainly don’t want to put anyone off getting an IUD as our review data shows that the Hormonal IUS and Copper IUD have the highest overall satisfaction rating of any contraceptive method. But it’s so important that we have access to the right information, advice and pain relief to make the fitting procedure more comfortable.

Weird periods and covid vaccines
As a community that regularly discusses periods it didn’t take long for you to start telling us about changes to periods you’d noticed following the Covid-19 vaccine. In an Instagram poll over two thirds of you said yes you had noticed a correlation – with you noticing your periods have been heavier, longer, lighter, more painful, later, earlier, or unexpected. This was in line with women’s reports to the MHRA (Medicines and Healthcare products Regulatory Agency) through the yellow card side effect reporting scheme. Most people who report a change to their period after vaccination find that it returns to normal the following cycle and, importantly, there is no evidence that Covid-19 vaccination adversely affects fertility.
We teamed up with Dr Victoria Male to answer all your questions on Covid vaccines, periods and fertility in an online webinar which loads of you attended. We discussed how:
- Changes to periods are common but not widely talked about or recognised. Changes can result from a variety of factors including undiagnosed underlying medical or gynaecological conditions, but also other things we may not realise such as exposure to stress, excessive exercise, eating disorders, changes in weight, depression and acute and chronic illnesses. Media scrutiny and sheer numbers of vaccinated women world wide mean we are now talking about this.
- Whilst the number of reports of period irregularities and vaginal bleeding is low in relation to both the millions of people who have received Covid-19 vaccines to date and how common menstrual disorders are generally, it is plausible that in some people the immune response to vaccination can trigger temporary changes to periods.
- The MHRA’s investigation and subsequent studies have been reactive as a result of women sharing experiences and expressing concern. We think this reflects a gender bias in clinical research trials and a lack of emphasis on the importance of reproductive health to women’s daily lives. The effects of medical interventions on periods should not be an afterthought in future research. This should also be a lesson on how we respond to the reporting of potential side effects, we must address what is important to women. Vaccine hesitancy among young women is largely driven by false claims that Covid-19 vaccines could harm their chances of future pregnancy. Failing to thoroughly investigate reports of menstrual changes after vaccination is likely to fuel these fears.We’d like to see menstrual irregularities investigated as part of clinical trials so women can be made aware of potential side effects, or reassured that they are not linked, and so they can be prepared rather than anxious or worried. Clear and trusted information is particularly important for those who rely on being able to predict their menstrual cycles to either achieve or avoid pregnancy.
We are obsessed with fertility
The issue of contraception and long term effects on fertility comes up time and time again and is a myth that is perpetuated. As we’ve seen with Covid-19 vaccines, concerns about fertility and medical interventions are not just limited to contraception. The stress, anxiety, stigma, fear and shame surrounding infertility means it’s at least a subconscious worry for many women.
Want the lowdown? Changes to periods are a common side effect of contraception, which does by its very nature, in the short term, affect your fertility to stop you getting pregnant. However in some women the benefits of contraceptive use, such as making periods less frequent or stopping them altogether, can mask an underlying problem that may affect fertility.
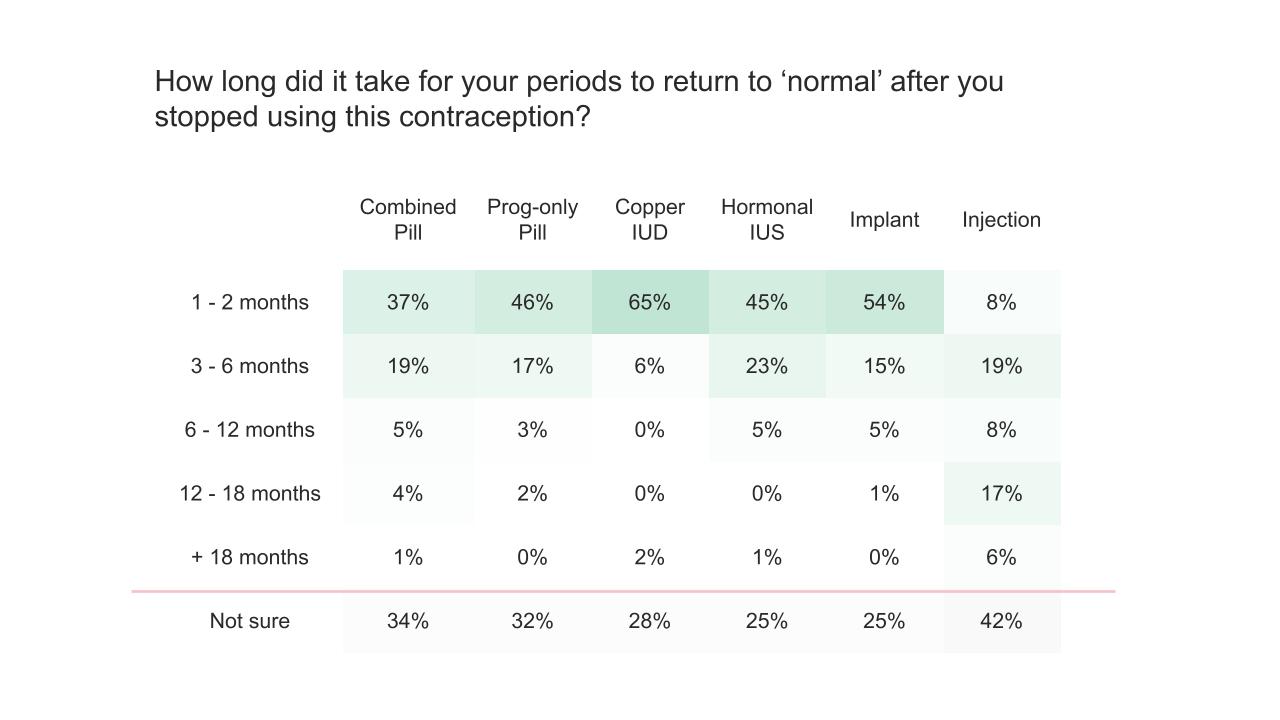
Of all reversible methods of contraception only the injection has the potential to cause a short term delay in return to fertility for up to 12-18 months after stopping, with no significant difference in pregnancy rates 2 years after stopping.
For all other methods of reversible and hormonal contraception, fertility returns to what is normal for you as soon as you stop your method of contraception. Research supported by real world data from The Lowdown reviews, shows most women see a return of their periods to what is normal for them a few months after stopping. In order to tackle fears and stop the spread of harmful myths we’ve aimed to address your worries by including ‘effects on fertility after stopping’ for all the contraception methods on our website and of course writing an amazing blog all about it.
Mood
Mood change is one of the biggest concerns users of hormonal contraception have. And can impact on a woman’s decision to continue or even correctly use a contraceptive method. And we get it. For every woman who tells us their heavy periods or horrendous PMS has been helped by the pill, there is another woman who can tell us about her mood swings and anxiety. And the research on what effects to expect, or who might be affected is patchy, contradictory and scary.
Even without experiencing a mood problem many women seek advice from us because they’ve heard about potential mood effects and having used contraception since their teenage years often say ‘I don’t know who I am off contraception’. Without good evidence, doctors have little to go on and little advice to give when considering options. Unfortunately this often translates into perceived dismissiveness by the medical profession.
Our data is quite negatively biased with lots of women reporting negative changes to their mood with all sorts of contraception. We’re mindful that lots of this data has been collected over the last couple of years of pandemic life, and also reflects a community who is questioning their experiences. It might be that the hormonal effects of contraception on mood are a minor cog in the wheel, but also potentially a tipping point for some.
It’s unlikely we will get answers from traditional research which studies large numbers of people as there are so many confounding factors for individuals – age, genetics, medical history, relationships, life stressors, to name a few. This is an example of where sharing the limits of medical knowledge and addressing problems individually helps to manage uncertainty.
Why ‘back-to-backing’ your pill is not just that thing you did before your girls holiday to Zante in 2010
There are also areas where we want to see medical advice catch up with the evidence. Explaining to women you can take the combined pill continuously or with shorter breaks should be the norm. There is no medical reason for having a break on the combined pill and an associated bleed every month, although as always personal choice is a big factor. Taking your pill continuously can reduce associated problems like heavy or painful bleeding, PMS symptoms, headaches and the whole inconvenience of bleeding when you don’t have to. It is also likely to increase the effectiveness of the pill through reducing the risk of ovulation from a missed pill. Win-win.
Whilst most medical professionals will be able to advise women of this benefit it still is not seen as the status quo. Until we change outdated prescription guidance and medication information leaflets to reflect this, women will still believe this is hearsay and may even think they are going against medical advice. We’ve created a guide to continuous pill taking as an authoritative source for women – read it to learn why periods on the pill aren’t ‘real’!
‘Over the counter’ pills
At The Lowdown we were very happy to hear that a couple of months ago the MHRA made two, relatively unknown brands, of the very safe and highly effective desogestrel progestogen-only pill (POP) available over the counter (OTC) without a prescription. The option to buy the POP over the counter at pharmacies will be a convenient and easy choice for many, but unfortunately does not address the wider problem of access to free contraception and a choice of options for everyone that wants it.
We would like to see all brands of the desogestrel POP available without a prescription and free of charge from a wide range of services and settings. Lovima and Hana come at a higher price point than other pills and we must be careful not to add barriers to access for those who already find accessing contraception difficult, especially under the guise of removing them.
We would also like to ensure that women are able to access information and advice so they are fully informed of the potential and expected side effects of the POP, including for example, irregular bleeding, mood changes and acne. These common problems can lead to women stopping or changing contraceptives, or taking them incorrectly, and being vulnerable to unintended pregnancies.
At The Lowdown we strongly believe in reproductive autonomy for everyone and the development of more contraceptive options including a male contraceptive is an important step towards this. Individuals and couples should be able to decide on a contraceptive method that fits their lifestyle and needs, and the development of the male contraceptive will allow men to more actively participate in this.
We need to recognise the importance of personal choice and personal experience and the desire to seek out and learn from others with similar stories, as well as from traditional studies and research. The need for The Lowdown, as a space to voice this, to normalise and validate experiences, as a way to access a breadth of information AND individualised care, is overwhelming. In our experience encouraging nuanced conversations around the benefits and downsides of contraception empowers women to make informed positive choices, rather than discouraging contraception use as some might fear.
Finally I just want to say how amazing and inspiring it is to work with such a passionate team and by extension a community of thousands of people who want to make each other’s lives better by improving women’s experiences of accessing and choosing contraception. This is clearly just the start of what’s to come!
Fancy talking to Dr Mel about your contraception? Book an appointment with her below!
Tags
- Lenger SM, Bradley MS, Thomas DA, Bertolet MH, Lowder JL, Sutcliffe S. D-mannose vs other agents for recurrent urinary tract infection prevention in adult women: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020 Aug;223(2):265.e1-265.e13. doi: 10.1016/j.ajog.2020.05.048. Epub 2020 Jun 1. PMID: 32497610; PMCID: PMC7395894.
- Kranjčec B, Papeš D, Altarac S. D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J Urol. 2014 Feb;32(1):79-84. doi: 10.1007/s00345-013-1091-6. Epub 2013 Apr 30. PMID: 23633128.
- NICE guideline [NG112] Urinary tract infection (recurrent): antimicrobial prescribing. 2018
- Royal College of Obstetricians and Gynaecologists. Long-term Consequences of Polycystic Ovary Syndrome, Green-top Guideline No. 33. Nov 2014.
- Siemienowicz K et al. Insights into Manipulating Postprandial Energy Expenditure to Manage Weight Gain in Polycystic Ovary Syndrome. iScience. 2020.
- Faculty of Sexual and Reproductive Health. FSRH Clinical Guideline: Intrauterine Contraception (April 2015, amended September 2019)
Dr Mel is a GP from London experienced in women’s health. Mel has worked in a sexual health clinic and has seen pretty much everything going! She knows all the latest research and helps us interpret the evidence behind contraception and fact checks our website and social content.